© 2025 MJH Life Sciences™ , Patient Care Online – Primary Care News and Clinical Resources. All rights reserved.
Treatment of Diabetes in Older Adults: Guideline Highlights
The Numbers: >90% of US adults aged ≥65 yrs have diabetes; 33% of those have T2DM; ~50% of older adults have prediabetes. We highlight new Endocrine Society treatment guidance.

Treatment of Diabetes in Older Adults: Highlights from An Endocrine Society Clinical Practice Guideline, J Clin Endocrinol Metab, May 2019
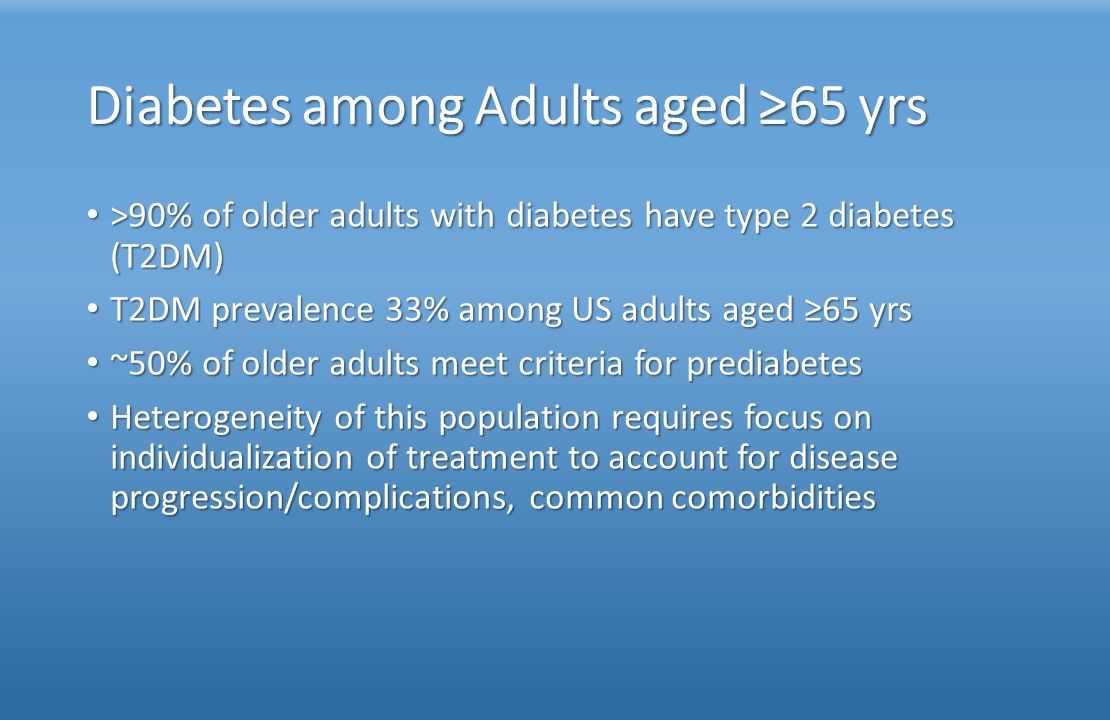
>90% of older adults with diabetes have type 2 diabetes (T2DM); T2DM prevalence is 33% among US adults aged ≥65 yrs; approximately half of older adults meet criteria for prediabetes. Heterogeneity of this population requires focus on individualization of treatment to account for disease progression/complications, common comorbidities.
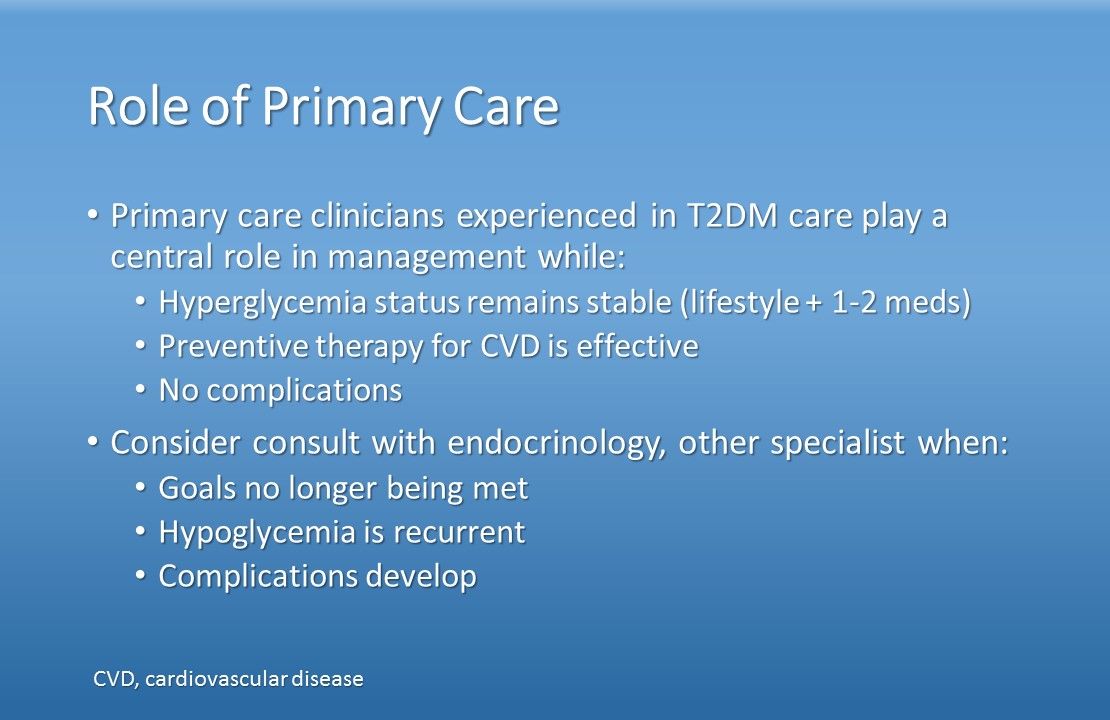
Primary care clinicians experienced in T2DM care play a central role in management while: Hyperglycemia status remains stable (lifestyle + 1-2 meds); preventive therapy for CVD is effective; the patient has no complications. Consider consult with endocrinology, other specialist when: Glycemic goals no longer being met; hypoglycemia is recurrent; complications develop.
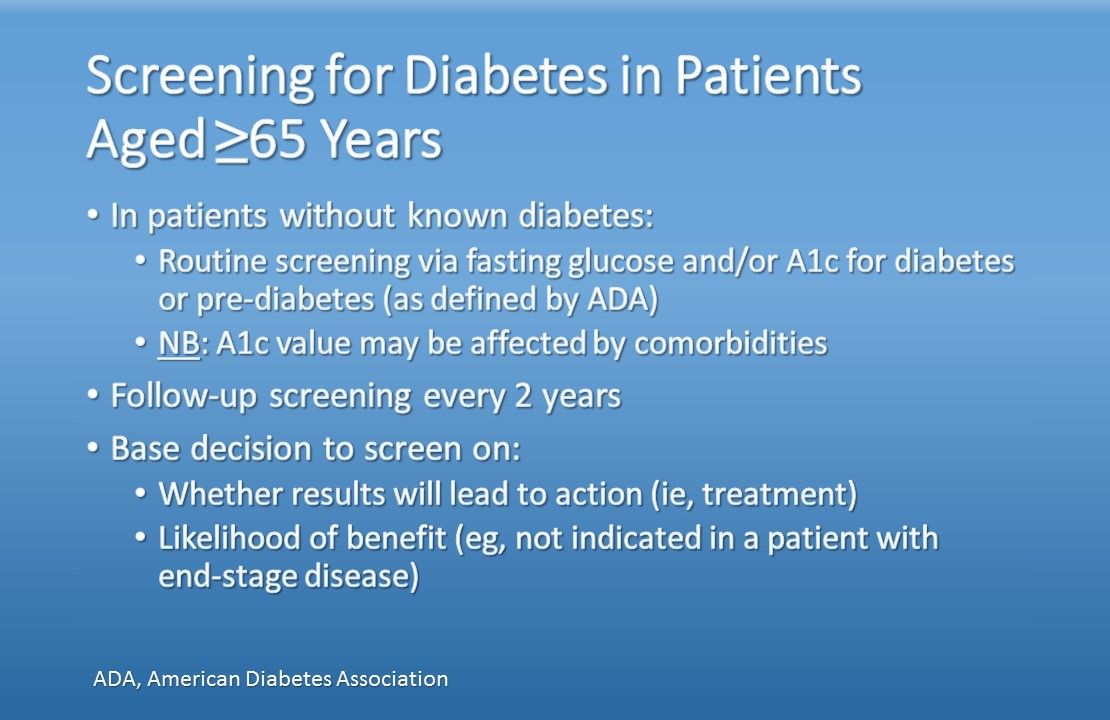
In patients without known diabetes: Routine screening via fasting glucose and/or A1c for diabetes or pre-diabetes (as defined by ADA). NB: A1c value may be affected by comorbidities; perform follow-up screening every 2 years. Base decision to screen on: Whether results will lead to action (ie, treatment); likelihood of benefit (eg, not indicated in a patient with end-stage disease).
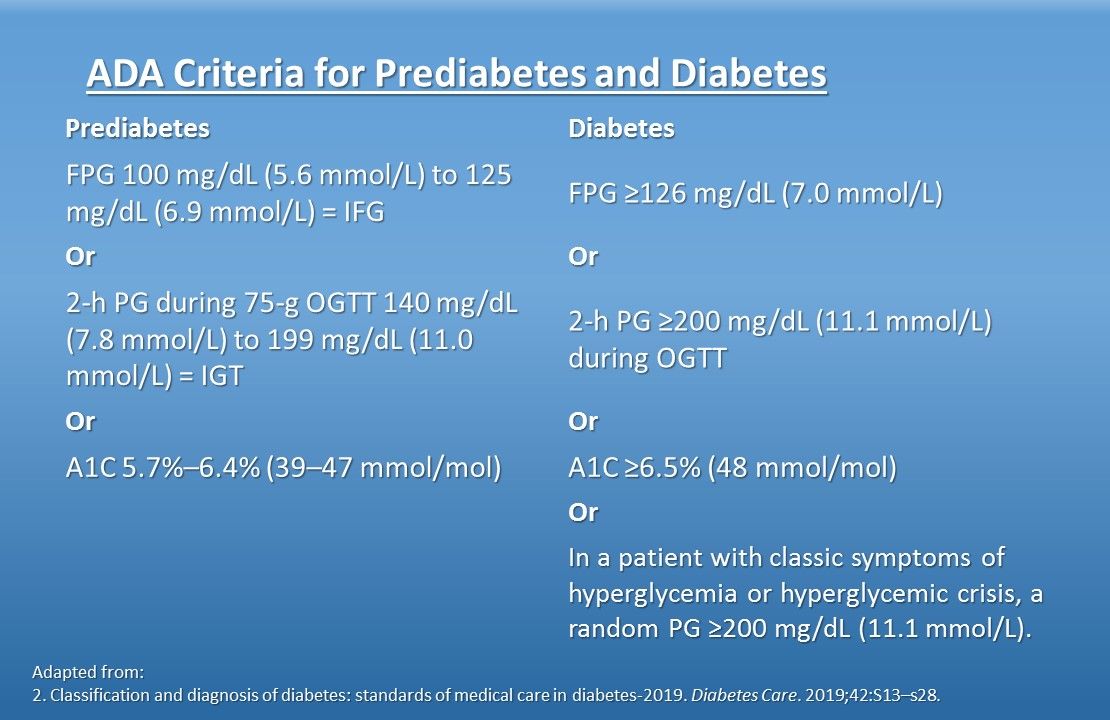
ADA Criteria for Prediabetes and Diabetes.
Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019 Jan; 42(Supplement 1):S1-S2.
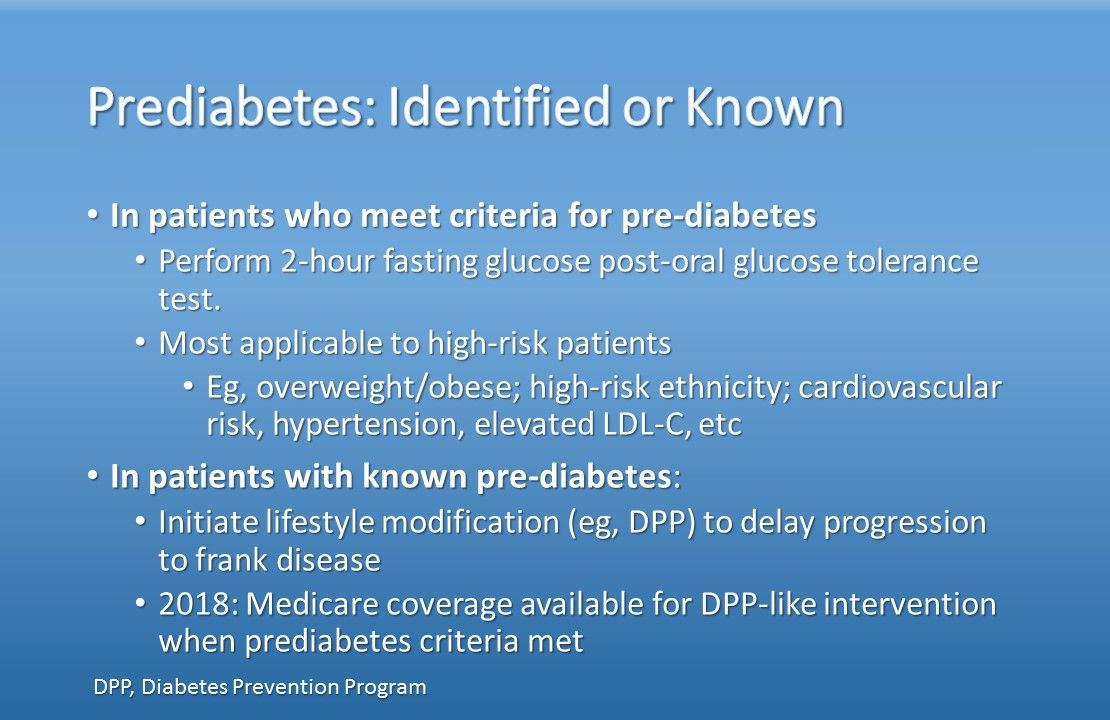
In patients who meet criteria for pre-diabetes: Perform 2-hour fasting glucose post-oral glucose tolerance test; this testing is most applicable in high-risk patients, eg, overweight/obese; high-risk ethnicity; cardiovascular risk, hypertension, elevated LDL-C, etc. In patients with known pre-diabetes: Initiate lifestyle modification (eg, DPP) to delay progression to frank disease. NB: 2018: Medicare coverage available for DPP-like intervention when prediabetes criteria met.
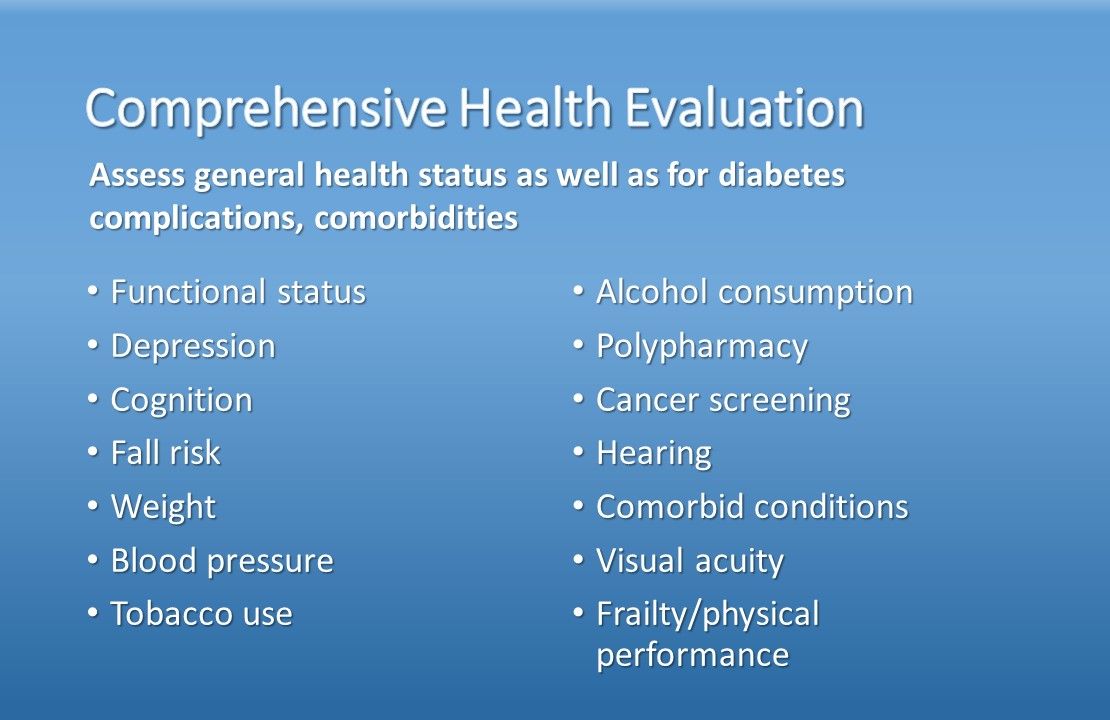
Assess general health status as well as for diabetes complications, comorbidities. Functional status, depression, cognition, fall risk, weight; blood pressure, tobacco use, alcohol consumption, polypharmacy, cancer screening, hearing, comorbid conditions, visual acuity, frailty/physical performance.
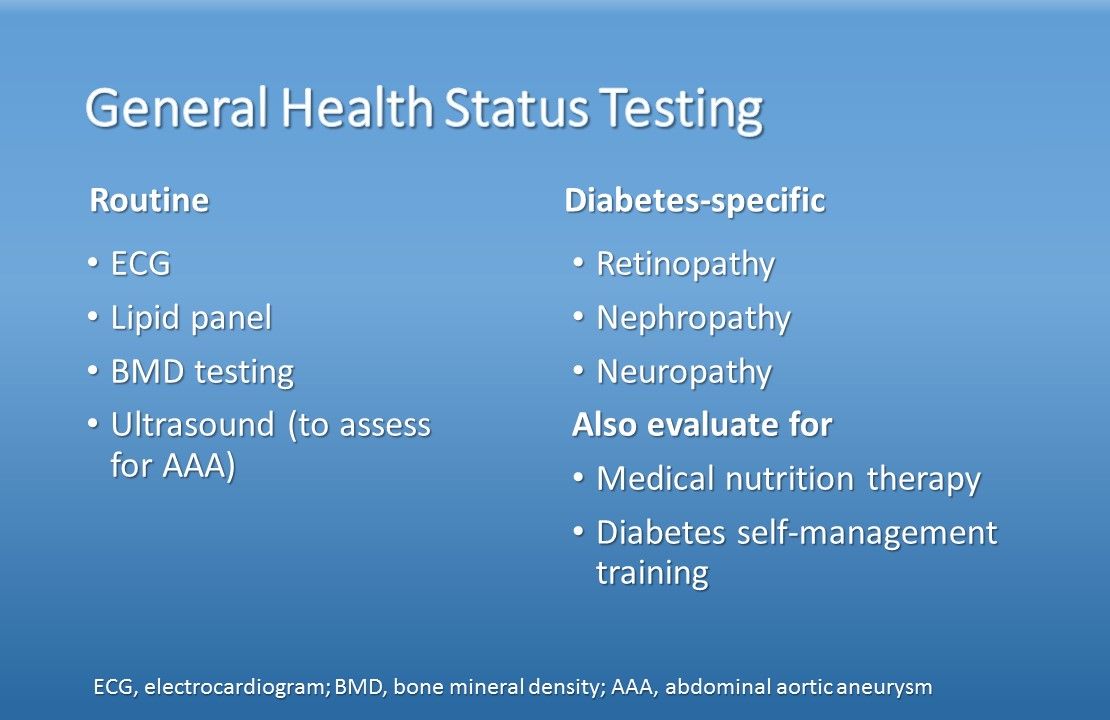
Conduct routine general health status testing: ECG, lipid panel, bone mineral density, ultrasound to assess for abdominal aortic aneurysm. Monitor diabetes-specific health: Retinopathy, nephropathy, neuropathy. Also evaluate for: Medical nutrition therapy, diabetes self-management training.
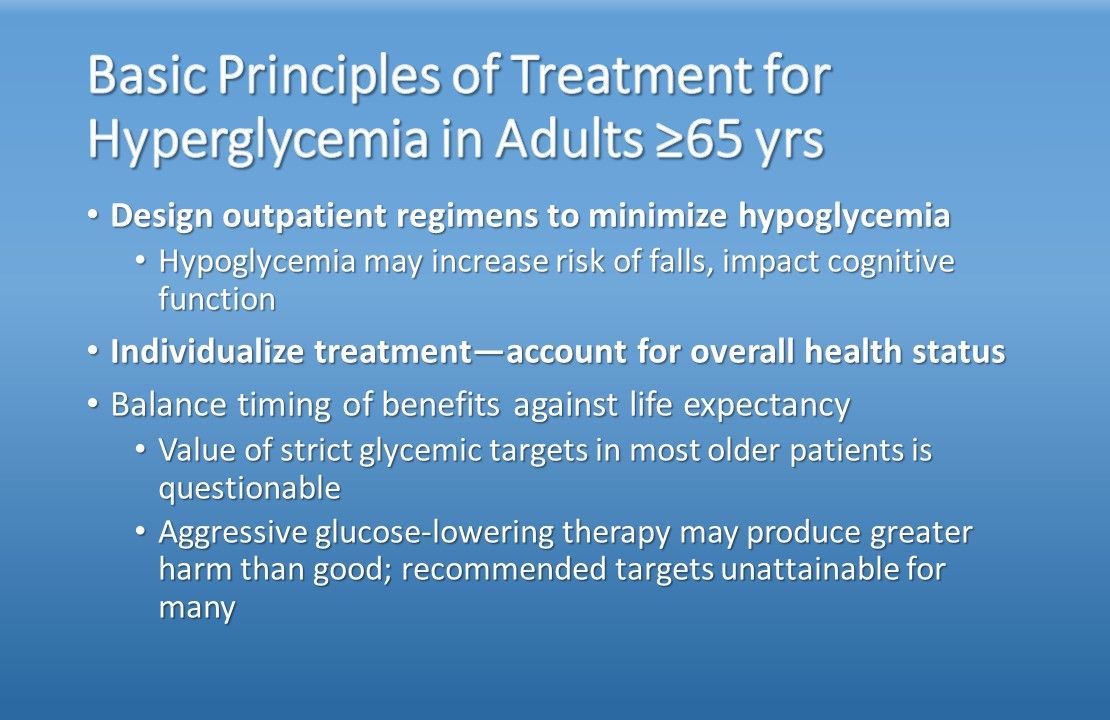
Design outpatient regimens to minimize hypoglycemia: Hypoglycemia may increase risk of falls, impact cognitive function. Individualize treatment-account for overall health status: Balance timing of benefits against life expectancy; value of strict glycemic targets in most older patients is questionable; aggressive glucose-lowering therapy may produce greater harm than good; recommended targets unattainable for many.
Nonpharmacologic management: Lifestyle modifications-first-line in ambulatory patients; assess nutrtional status to detect malnutrition, continue nutrition management; address frailty with high-protein diet; if glycemic targets can’t be met with lifestyle change, limit simple sugars; forgo restrictive dieting; closely monitor glycemic response to dietary changes.
Pharmacologic management: Adjust glycemic management strategies to individual needs, health status, including comorbidities; keep regimens simple. Metformin is first-line oral Rx (contraindications-impaired renal function, GI intolerance). After metformin, add other oral/injectable agents and/or insulin as needed and based on other specific indications (eg, CV protection, weight loss, renal insufficiency): SUs, glinides, TZDs, α-glucoside inhibitors, DPP-4 and SGLT2 inhibitors, GLP-1 receptor agonists.
Manage macrovascular complications. Hypertension: target 140/90 mm Hg; hyperlipidemia: annual lipid profile; congestive heart failure, follow practice guidelines; atherosclerosis: aspirin for secondary prevention. Manage microvascular complications: Vision loss-retinopathy: annual comprehensive eye exam; neuropathy, falls, problems of lower extremities: fall risk precautions; physical therapy; vascular specialist; chronic kidney disease: annual screening; limit use/dosage of specific Rx.
Treating diabetes in special settings. Prevalence of diabetes in long-term care now at 35%. In hospitals/nursing homes: set clear inpatient glycemic targets; ensure explicit discharge plan to reestablish treatment targets, medications during transition. Simplify glycemic management in patients with severe comorbidities, terminal illness. Screen A1c routinely in older hospitalized patients without diabetes.

Transitions of care can be problematic. Most essential element: ongoing communication between discharge and receiving healthcare teams, discharge team and patient/family or caregiver. Patient newly diagnosed in hospital presents additional challenges. Comorbidities, cognitive and functional status will determine timing and specific steps in any transition.
The increased prevalance of type 2 diabetes in US adults is particulary notable in adults aged â¥65 years. Just as the aging process worsens the underlying pathophysiology of diabetes, the effects of aging also may accelerate the appearnce and progression of many common diabetes complications. Many principles of care for older adults with diabetes are the same as for younger persons with the disease; there are important diversions, however, which are clearly laid out in the "Treatment of Diabetes in Older Adults: An Endocrine Society Clinical Practice Guideline." The short slide show below summarizes main areas of focus.Â



