© 2025 MJH Life Sciences™ , Patient Care Online – Primary Care News and Clinical Resources. All rights reserved.
Reduce COPD Exacerbations with Combination Therapy
Combination therapy found to reduce COPD exacerbations, no exacerbation reduction with β-blockers, plus 3 more must-read studies.
Combination therapy reduces exacerbations. For patients who have severe COPD with chronic bronchial infection resulting from Pseudomonas aeruginosa, combination therapy with nebulized colistin and continuous cyclic azithromycin significantly reduced COPD exacerbations and P. aeruginosa sputum isolates. After 2 years of follow-up, exacerbations were reduced 38.3% from baseline, P. aeruginosa COPD exacerbations were reduced from 59.5% to 24.6%, and the P. aeruginosa eradication rate was 28%. The study was published online on October 17 in the International Journal of Chronic Obstructive Pulmonary Disease.
No exacerbation reduction with β-blockers. β-blockers do not reduce the risk of exacerbations and death in patients with moderate or severe COPD who did not have an established indication for β-blocker use. In a prospective, randomized trial of 532 patients, there was no significant between-group difference in median time until first exacerbation for patients who received metoprolol or placebo (202 days vs 222 days, respectively). Metoprolol was associated with a higher risk of exacerbation that leads to hospitalization (hazard ratio, 1.91; 95% CI, 1.29-2.83). The study was published on October 20 in the New England Journal of Medicine.
Care program did more harm than good. In a corrected version of a 2018 article, a 3-month program that combined transitional care and long-term self-management support for patients hospitalized with COPD led to more hospitalizations and ED visits, not fewer as originally reported. Compared with the usual care group, the intervention group had 1.40 COPD-related acute care events/participant vs 0.72 (usual care group) and a mean change in SGRQ total score of 2.81 vs −2.69 at 6 months. There was no improvement in QoL. The republished study appeared in JAMA on October 8.
Bronchodilator testing prevents overdiagnosis. When spirometry is not combined with bronchodilator testing, there is almost a 40% chance of COPD overdiagnosis, and asthma and asthma-COPD overlap syndrome may be missed, according to study findings presented at the CHEST Annual Meeting 2019 in October. Of the 625 subjects from the National Health and Nutrition Examination Survey data who met American Thoracic Society spirometry quality standards and had airway obstruction based on prebronchodilator FEV1/FVC ratio <0.7, only 61% continued to present an airway obstruction after bronchodilator testing.
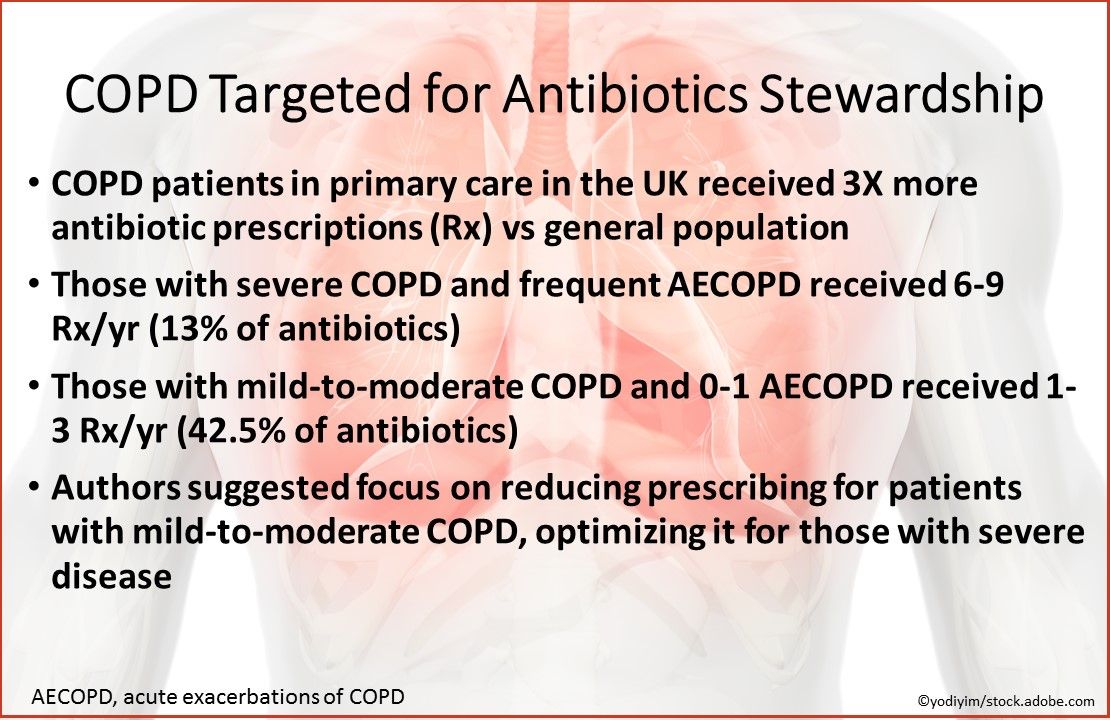
COPD targeted for antibiotics stewardship. In a UK study, patients with COPD in primary care received 3 times more antibiotic prescriptions vs the general population. Those with severe COPD and frequent AECOPD received 6-9 prescriptions/year (13% of antibiotics); those with mild-to-moderate COPD and 0-1 AECOPD received 1-3 prescriptions/year (42.5% of antibiotics). The authors suggested antibiotic stewardship should focus on reducing prescribing for patients with mild-to-moderate COPD and optimizing it for those with severe disease who are at risk of drug resistance. The study was published on October 9 in the Journal of Antimicrobial Chemotherapy.
Stay in touch with Patient Care® Online:
→Subscribe to ourNewsletter →Like us on Facebook →Follow us on Twitter →Write or Blog for Patient Care® Online→Follow us on LinkedIn
Combination therapy reduces exacerbations, no exacerbation reduction with beta-blockers, care program did harm rather than good-these are some of the latest developments in chronic obstructive pulmonary disease (COPD) research. Scroll through the slides below to find concise summaries of key points for clinical practice.




