© 2025 MJH Life Sciences™ , Patient Care Online – Primary Care News and Clinical Resources. All rights reserved.
Quality of Life Factors in Behçet Disease
In Behçet disease, disease activity and manifestations can significantly impact quality of life; lifestyle choices also play a role. We highlight 8 studies to help illustrate.
The disease activity and manifestations of Behçet disease (BD) may have a considerable impact on patients’ quality of life.
The onset, disease course, and the severity of inflammation in patients with BD may be influenced by a variety of lifestyle factors.
Scroll through the slides below for 8 concise descriptions of research on key quality of life factors in BD.
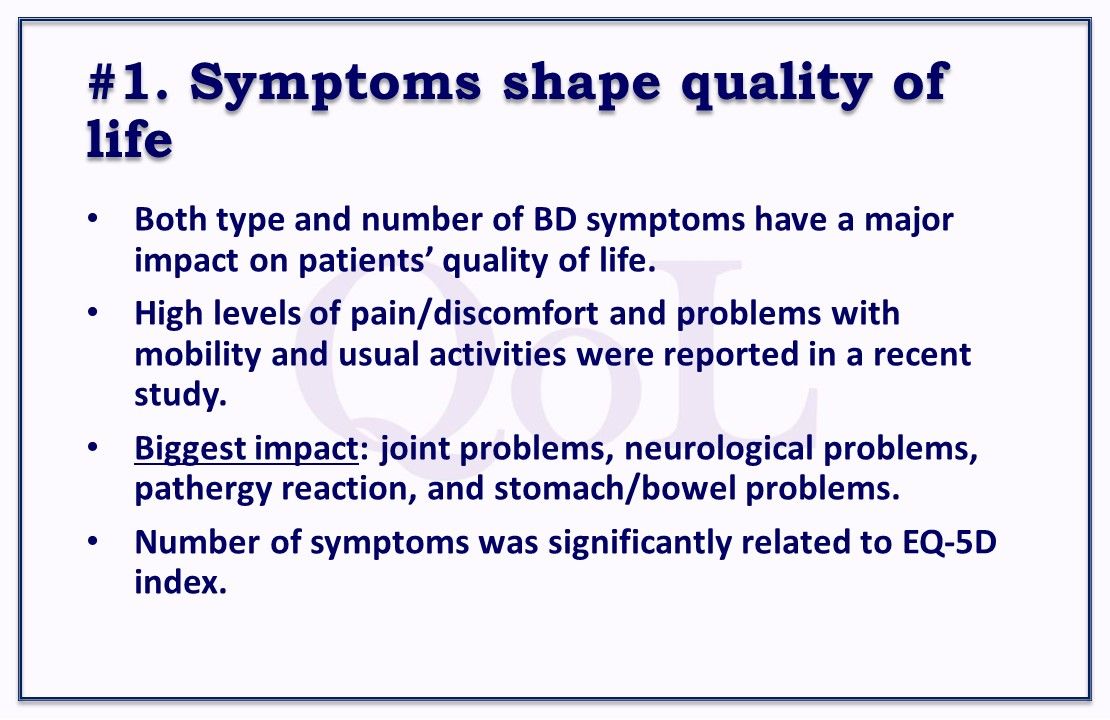
Symptoms shape quality of life. Both the type and number of BD symptoms have a major impact on patients’ quality of life, authors found. Study patients reported high levels of pain/discomfort and problems with mobility and usual activities. Of 10 assessed symptoms, joint problems had the biggest impact, followed by neurological problems, pathergy reaction, and stomach/bowel problems. The number of symptoms was significantly related to the EQ-5D index. Rheumatology.
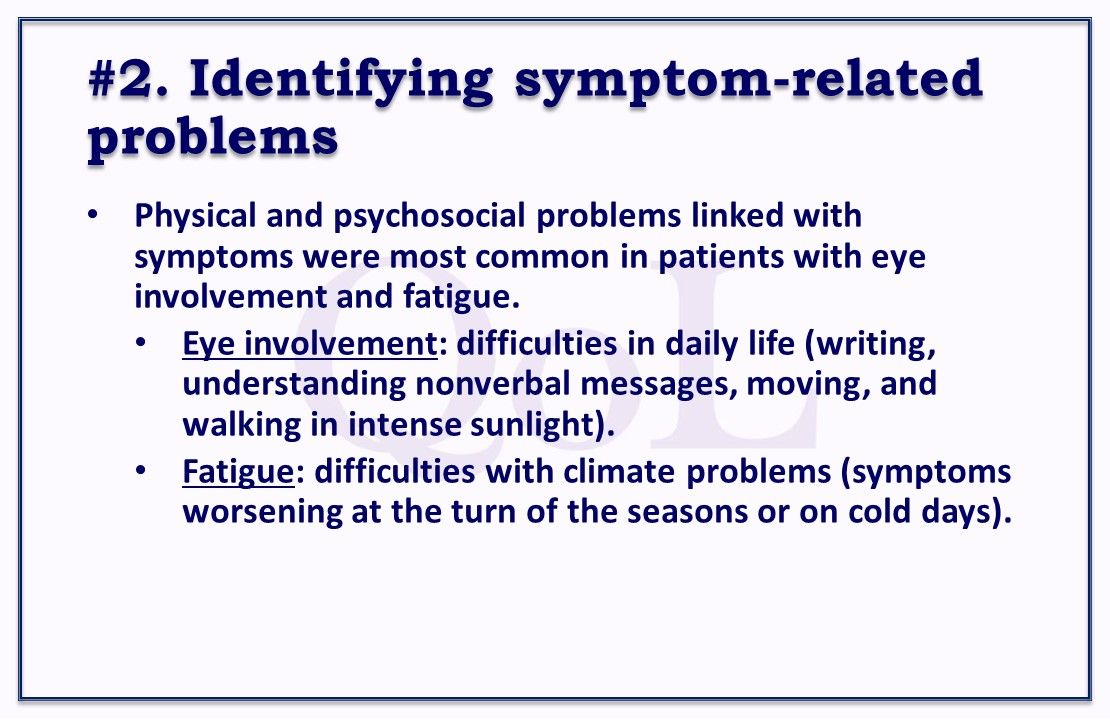
#2.Identifying symptom-related problems. Physical and psychosocial problems linked with symptoms were most common in patients with eye involvement and fatigue. Those with eye involvement had difficulties in daily life—writing, understanding nonverbal messages (eg, gestures and facial expressions), moving, and walking in intense sunlight. Those with fatigue had difficulties with climate problems—symptoms worsening at the turn of the seasons or on cold days. Rheumatology International.
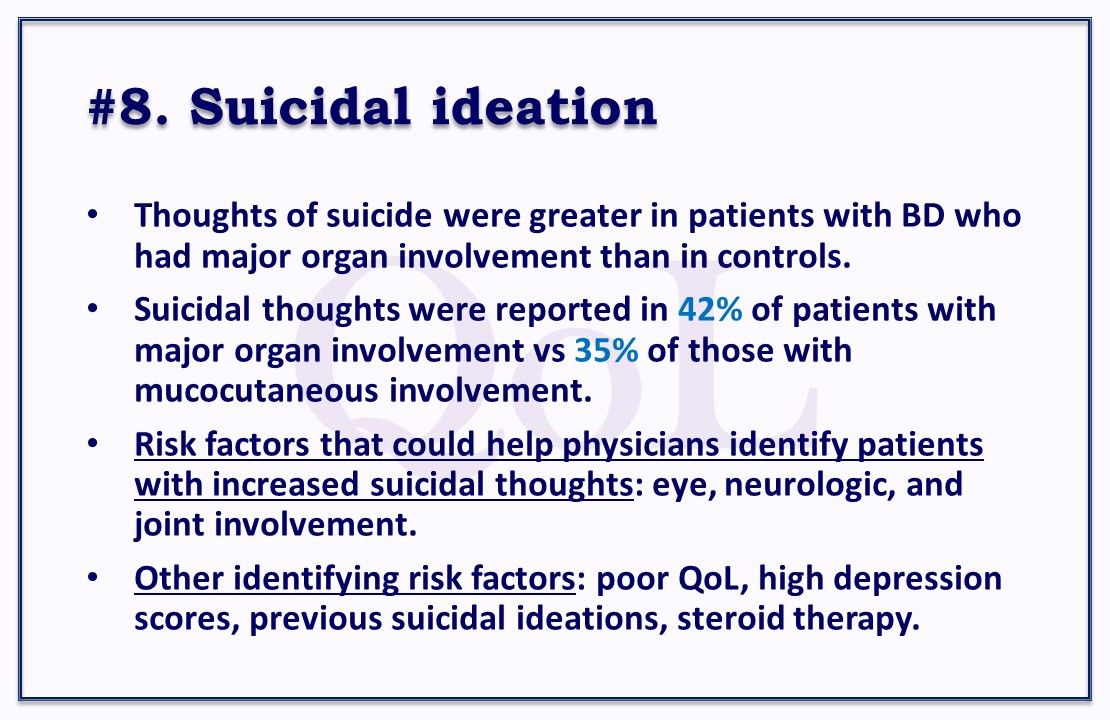
#3. If sleep suffers. The biggest factor patients with BD associated with low wellness and health status in a recent study was sleep quality. They began to feel significantly lower wellness and health status if just one-third of sleep quality was disrupted. Top disruptions were difficulty falling asleep, waking too early, snoring, excessive daytime sleepiness, and feeling tired upon waking in the morning. Also, mood status was almost significantly associated with self-rated wellness and health status. BMC Rheumatology.

#4. Low physical activity levels. In the first study to evaluate physical activity in patients with BD, activity levels were significantly lower in patients with BD than in healthy peers. Of patients with BD, 53.7% had low levels and 46.3% had moderate levels. Of healthy subjects, 9.1% had low levels, 47% moderate levels, and 43.9% high levels. Decreased physical activity may be linked with the pain and fatigue often seen in patients with BD—86.6% reported pain and 73.1% fatigue. Annals of the Rheumatic Diseases.
#5. Top triggers for oral ulcers. Close to two-thirds of study patients with BD reported external triggers for their oral ulcer recurrences. The most common specific factor: stress/fatigue (37%-47% of patients). Second most common: food, in particular, tree nuts, cheese, citrus fruits, pineapple, and strawberries (32%-35% of patients). Mechanical and hormonal factors also were cited. The authors suggested considering these external factors in the management of oral ulcers. Arthritis Care & Research.
#6. Smoking risk analysis. Ever smoking was not significantly associated with an increased risk of BD compared with never smoking in a case-control study. The relative risk of BD was 0.8–2.6 compared with healthy siblings and healthy unrelated persons. Although no significant differences in ever smokers and never smokers were observed in the clinical manifestations of patients with BD, disease activity at presentation was significantly greater in ever smokers. Modern Rheumatology.
#7. Lifestyle, employment, and education. Health-related lifestyles and employment status may have a significant impact on health related quality of life in patients with BD. In this study, tobacco use had a negative effect; mouthwash use had a significant positive effect. Mean EQ-5D was better in patients who continued in employment and were not receiving benefits. EQ-5D also was significantly higher in patients with a high level of education attainment. Clinical and Experimental Rheumatology 2017.