© 2025 MJH Life Sciences™ , Patient Care Online – Primary Care News and Clinical Resources. All rights reserved.
Medical Sequelae Impact QoL Among Individuals in Recovery
More than one-third of those in recovery from drug/alcohol use have chronic physical disease. A novel study looks at prevalence of health issues by type of substance used.

“… more than one-third of those who consider themselves in recovery from an alcohol or other substance use disorder continue to suffer from chronic physical disease.”
Alcohol, Substance Use Disorders in the US.1According to the National Survey on Drug Use & Health ~20 million in US (≥12 yrs) battled substance use disorder in 2017; ~ 74% of adults suffering from a substance use disorder in 2017 struggled with an alcohol use disorder; ~38% of adults in 2017 battled an illicit drug use disorder; 1 out of 8 adults struggled in 2017 with alcohol and drug use disorders simultaneously.
Addiction Recovery in the United States.2 ~ 9% of US adult population has resolved a significant alcohol and other drug (AOD) problem; but the burden of addiction does not end with "putting down" the substance.
Into Recovery, but Not out of the Woods. Medical, psychiatric sequelae of AOD persist with extensive personal, social, economic consequences; there is little research into the health status of adults in recovery from AOD. This study3 investigated prevalence of medical conditions caused/exacerbated by chronic AOD exposure to better understand lifetime disease burden of AOD use.
Substances and Sequelae. Nationally representative sample of >2000 US adults; incorporated data from 2017 National Recovery Survey. Weighted lifetime prevalence of common conditions estimated/compared to NHANES national averages. Disease prevalence examined across substances to account for medical issues specific to exposure. Demographic/clinical correlates of disease prevalence and relationship between distinct conditions/QOL explored.
Substances, Clinical Correlates. Substances: Alcohol, cannabis, cocaine, methamphetamine, opioids, stimulants, other drugs. Clinical corrleates: 1° substance used, age of onset of regular use, # substances used ≥10 times, years since AOD resolution, # yrs smoked (lifetime), outpatient, inpatient, residential treatment (yes/no), mutual help meetings, happiness, self-esteem, QOL, psychological distress.
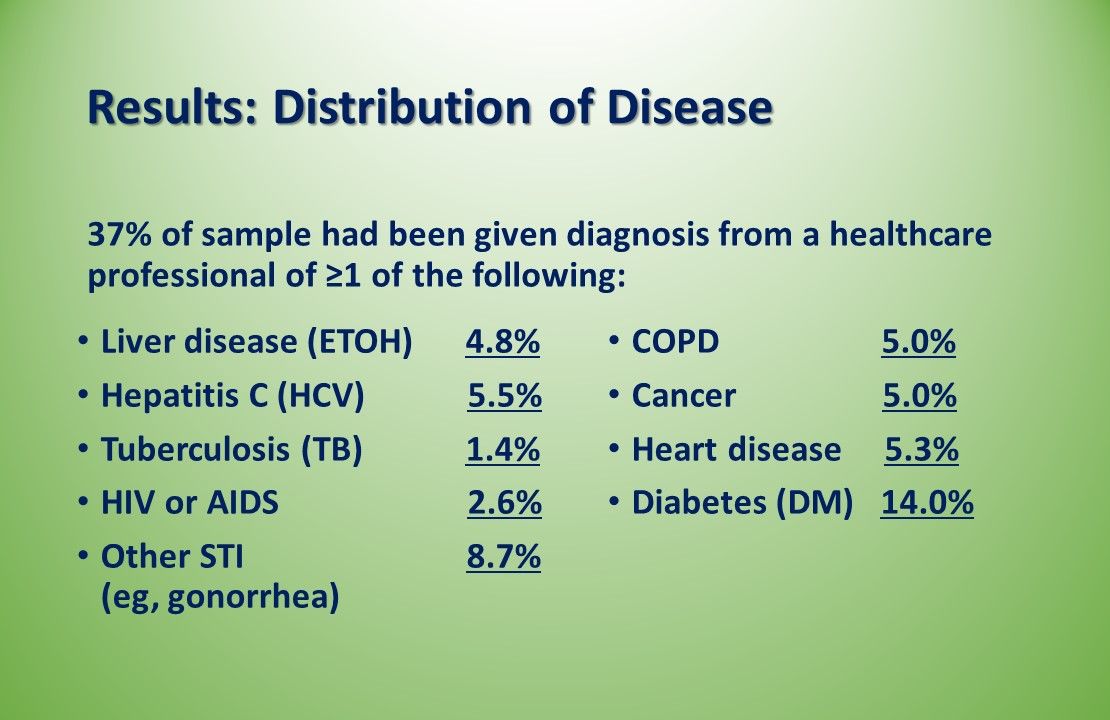
Results: Distribution of Disease. More than one-third (37%) of sample had been given a diagnosis from a healthcare professional of ≥1 of the disesaes above: Alcohol related liver disease, hepatitis C, tuberculosis, HIV or AIDS, another STI, COPD, cancer, heart disease, diabetes.
Disease Prevalence by Primary Substance. Liver disease (ETOH): Highest in ETOH use, but only slightly higher than in opioids/stimulant use; also increased prevalence in cannabis group. Hep C: Significantly higher in opioid, stimulant users vs ETOH users. Lifetime HIV/AIDs, other STIs: Significantly higher in stimulant vs ETOH group. Heart disease: Most common in the primary ETOH group. Cancer, TB, COPD: No significant differences among primary substance use groups.

Correlates of Physical Conditions. Current employment associated with lower odds of liver disease (ETOH), HIV/AIDS, COPD, cancer, heart disease, diabetes. Older age related to elevated odds of COPD, cancer, heart disease, diabetes. BA degree or higher, lower odds of COPD, HCV, HIV/AIDS, diabetes vs no HS diploma. Females less likely to report liver disease (ETOH), HCV, cancer, heart disease, diabetes but more likely to have had STI.
Demographic Correlates. Having at least high school diploma associated with ~ 60% reduced odds of having chronic disease in recovery. Having few/no chronic physical diseases in recovery associated with characteristics including younger age, being employed, being female, Hispanic race.
Clinical Correlates. Increased odds of ≥2 chronic physical diseases associated with: Each additional substance used ≥10 times, older age at disease onset, resolving AOD problem later in life.
Quality of Life. No lifetime history of medical condition, better QoL; liver disease (ETOH), COPD, diabetes significantly associated with lower QoL; liver disease (ETOH), TB associated with greater psychological distress; having cancer at any time significantly associated with better QoL scores.
Study Limitations. Cross sectional data reflect lifetime disease occurrence; disease may predate AOD problem; screening, access to medical care/insurance not retrospectively assessed; potential impact unknown; specific parameters of an AOD problem subjective, determined by participant; large sample size but prevalence of some medical conditions quite low; study possibly underpowered; but, tests multiple bivariate associations, increasing risk of type 1 error.
Summary/Take Home Points
- First study to document national prevalence estimates of common physical diseases among those who have resolved AOD problem
- Findings indicate greater lifetime physical disease burden among these persons vs general, noninstitutionalized US population
- Sex and primary substance used appear to influence likelihood of having a lifetime diagnosis
- Compared with age-standardized national lifetime prevalence rates Hep C, COPD, heart disease, diabetes significantly more prevalent in NRS sample
Author's Observations. Lead author David Eddie, PhD, from the Center for Addiction Medicine, Massachusetts General Hospital, Harvard Medical School notes that earlier intervention in the alchohol and substance use pattern may help prevent or mitigate these chronic conditions. He emphasizes that "...addiction treatment needs to be more seamlessly integrated with primary health care, and more research is needed to explore the complex relationships between alcohol and other drug use and physical disease.”
References
1. Statistics on Drug Addiction. American Addiction Centers Web site. https://americanaddictioncenters.org/rehab-guide/addiction-statistics. Accessed April 1, 2019.
2. Kelly JF, Bergman B, Heoppner BB, Vilsaint C, White WL. Prevalence and pathways of recovery from drug and alcohol problems in the United States population: Implications for practice, research, and policy. Drug, Alcohol Dep. 2017;181:162-169.
3. Eddie D, Greene MC, White WL, Kelly JF. Medical burden of disease among individuals in recovery from alcohol and other drug problems I the United States: findings from the national recovery survey. J Addict Med. 2019. In press.
In 2017, 19.7 million American adults battled a substance use disorder and 1 out of every 8 adults struggled with concomitant alcohol and drug use disorders.1 And while 9% of US adults has resolved a significant alcohol/drug problem,2 more than one-third of them have persistent health problems.3 David Eddie, PhD, at the Recovery Research Institute, Center for Addiction Medicine, Massachusetts General Hospital, Harvard Medical School and colleagues writing in the March issue of Journal of Addiction Medicine, report results of their novel study that examined which health issues appear to be associated with which type of abuse as well as the clinical and demographic correlates. Click through study highlights, below.Â
Related Content:




