© 2025 MJH Life Sciences™ , Patient Care Online – Primary Care News and Clinical Resources. All rights reserved.
Issues in Insulin Management: 3 Cases of Type 2 Diabetes
Three patients with type 2 diabetes in different stages of life and disease all require insulin management for A1c control.
Three patients present to you for type 2 diabetes follow-up care in different stages of disease progression and at different levels of treatment with insulin. Should regimens be changed? Should insulin be swapped out? What is the 2020 American Diabetes Assocation Standards of Medical Care recommendation for each patient? See what you think.
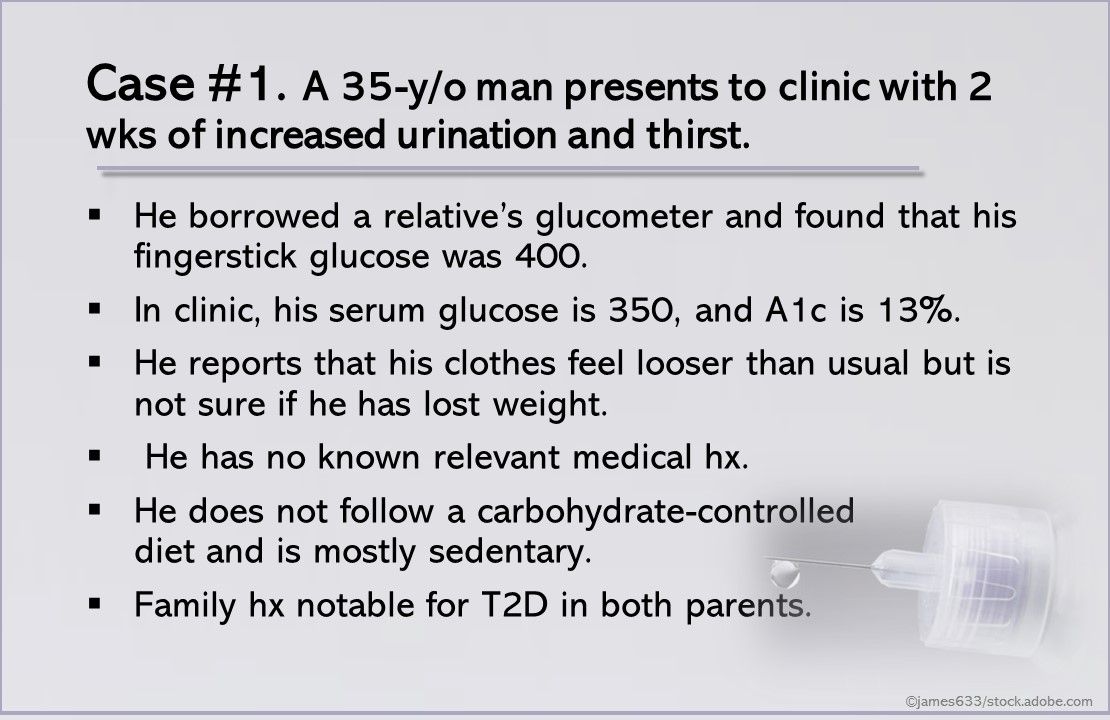
Case #1. A 35-year-old man presents to clinic with 2 weeks of increased urination and thirst. He borrowed a relative’s glucometer and found that his fingerstick glucose was 400. In clinic, his serum glucose is 350 mg/dL, and his A1c is 13%. He also reports that his clothes feel looser than usual but is not sure if he has lost weight.
He has no known medical history. He does not follow a carbohydrate-controlled diet and is mostly sedentary. His family history is notable for type 2 diabetes in both parents.
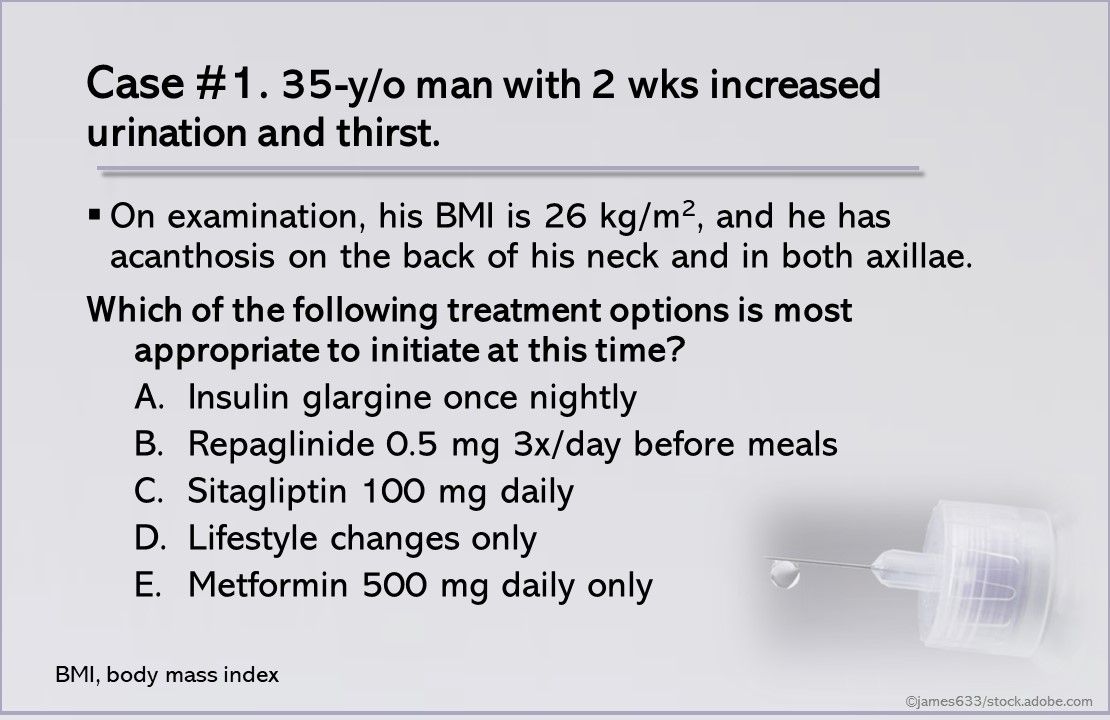
Case #1. 35-y/o man with 2 wks increased urination and thirst. Which of the treatment options above should be initiated at this time?
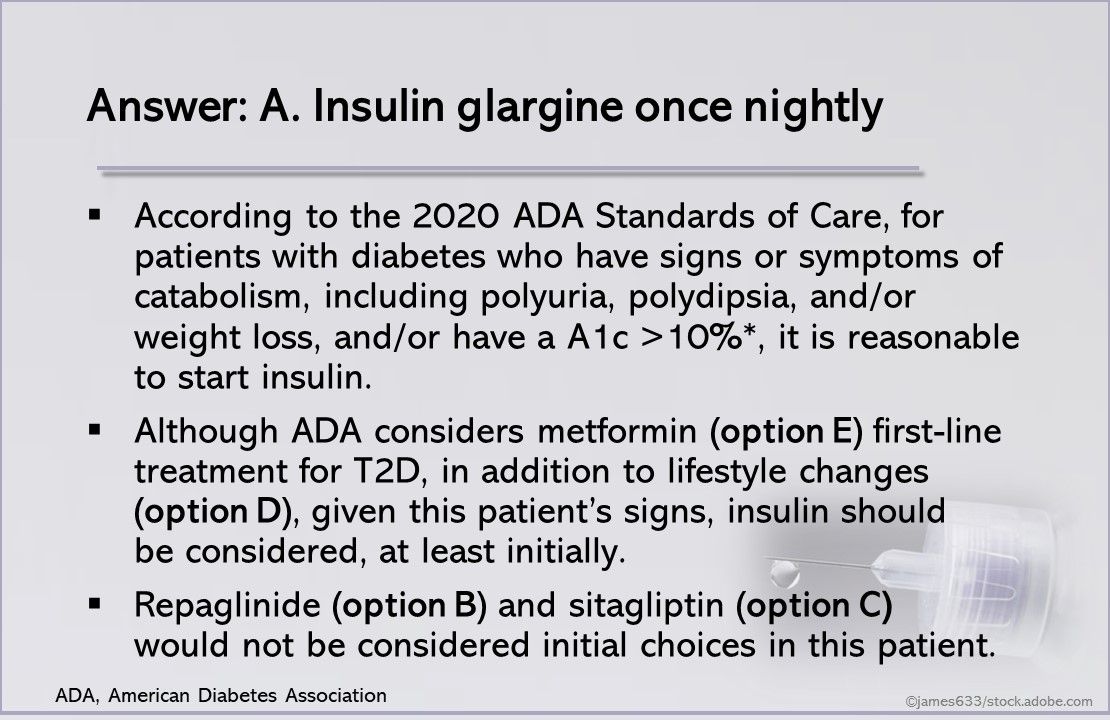
Answer: A. Insulin glargine once nightly. According to the 2020 American Diabetes Association (ADA) Standards of Care, for patients with diabetes who have signs or symptoms of catabolism, including polyuria, polydipsia, and/or weight loss, and/or have a hemoglobin A1c >10%, starting insulin is reasonable (level of evidence E, which indicates expert consensus or clinical experience).
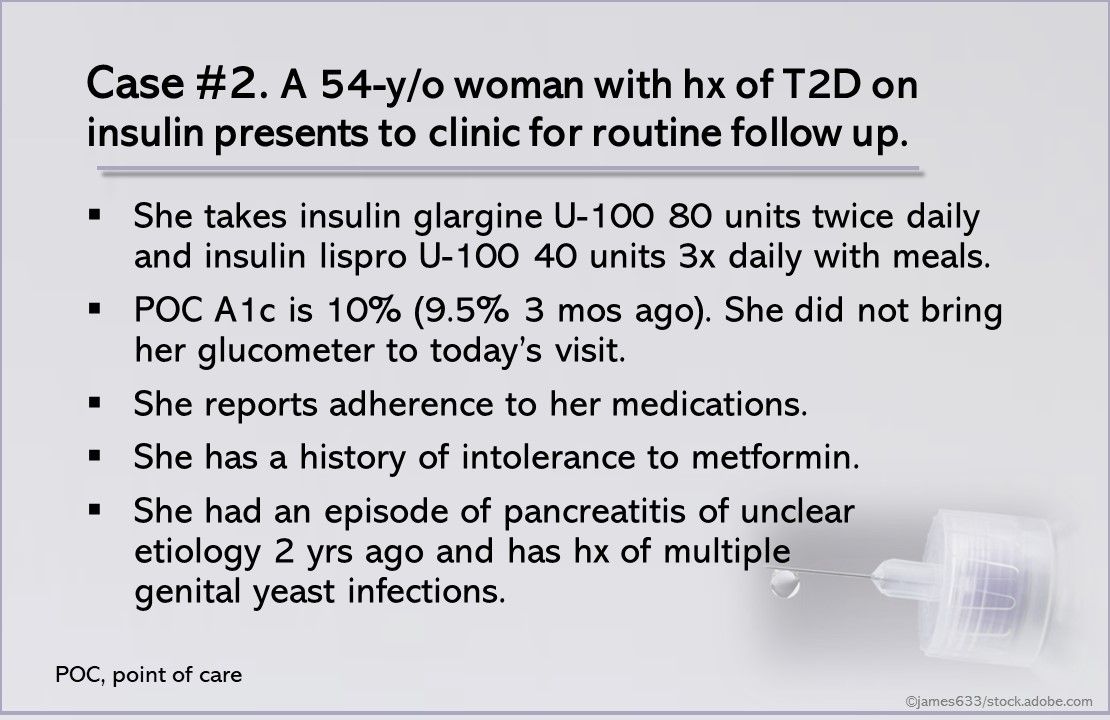
Case #2. A 54-year-old woman with a history of T2D on insulin presents to clinic for routine follow up of diabetes. She takes insulin glargine U-100 80 units twice daily and insulin lispro U-100 40 units 3 times daily with meals. Her point-of-care hemoglobin A1c is 10% (A1c 3 months ago was 9.5%).
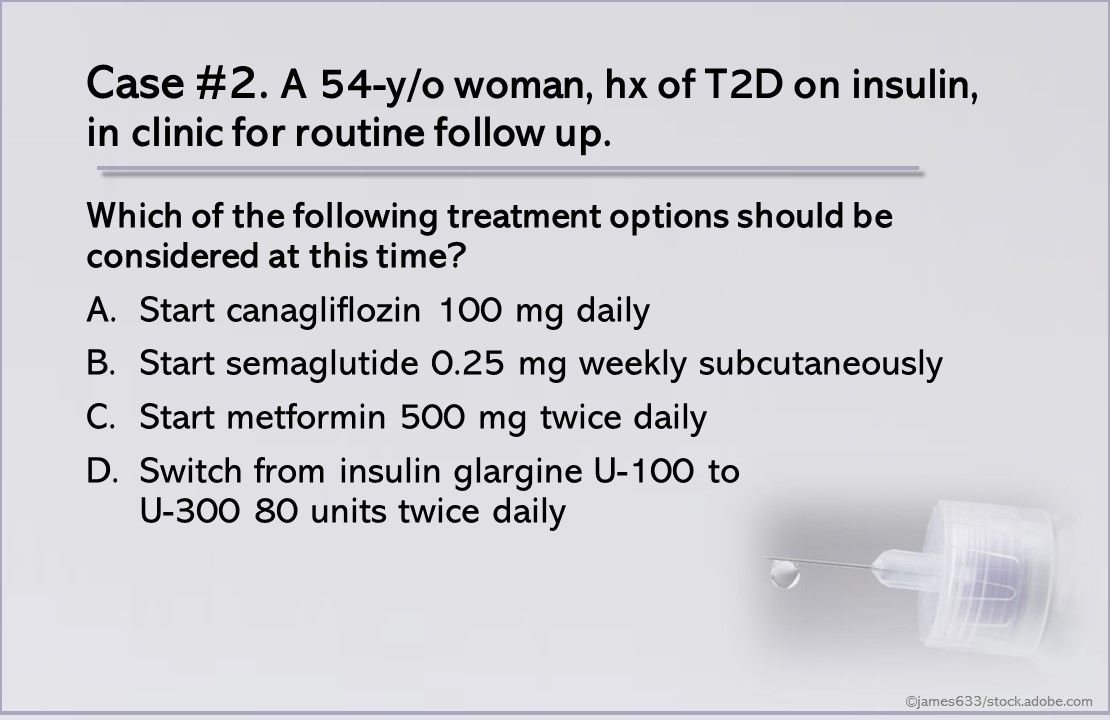
Case #2. A 54-year-old woman with a history of T2D on insulin presents to clinic for routine follow up of diabetes.
Which of the treatment options above should be considered?
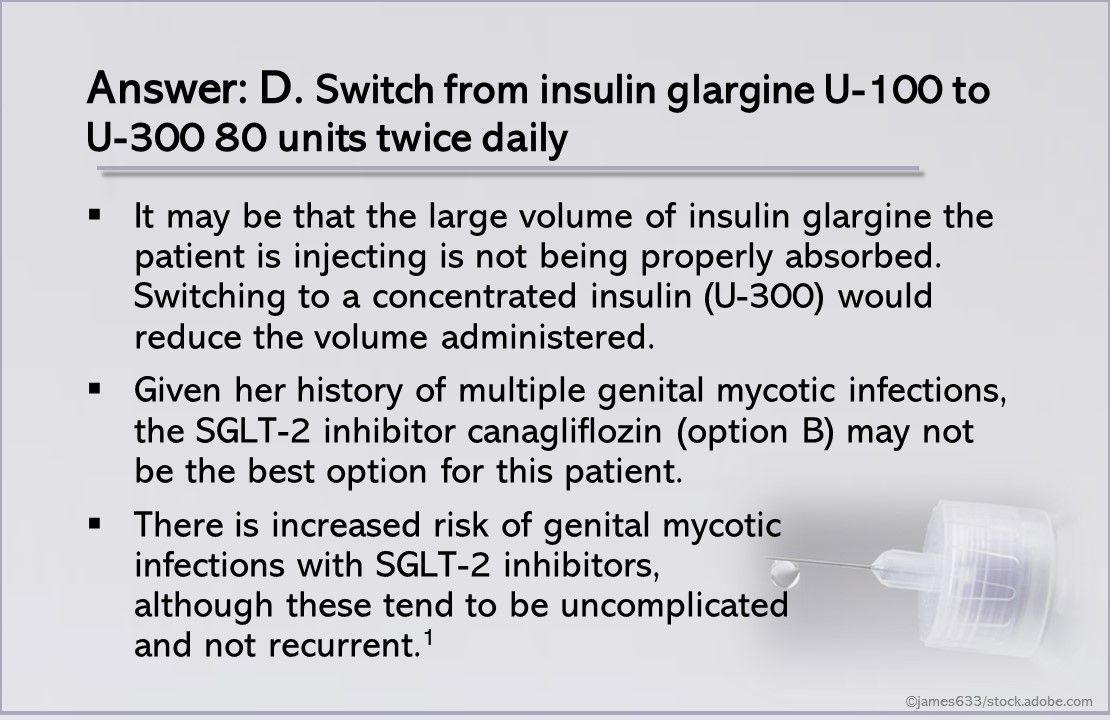
Answer: D. Switch from insulin glargine U-100 to U-300 80 units twice daily. It may be that the large volume of insulin glargine the patient is injecting is not being properly absorbed. Switching to a concentrated insulin (U-300) would reduce the volume administered.
1. Das SR, Everett BM, Birtcher KK, et al. 2018 ACC Expert Consensus Decision Pathway on Novel Therapies for Cardiovascular Risk Reduction in Patients With Type 2 Diabetes and Atherosclerotic Cardiovascular Disease: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2018;72:3200-3223.
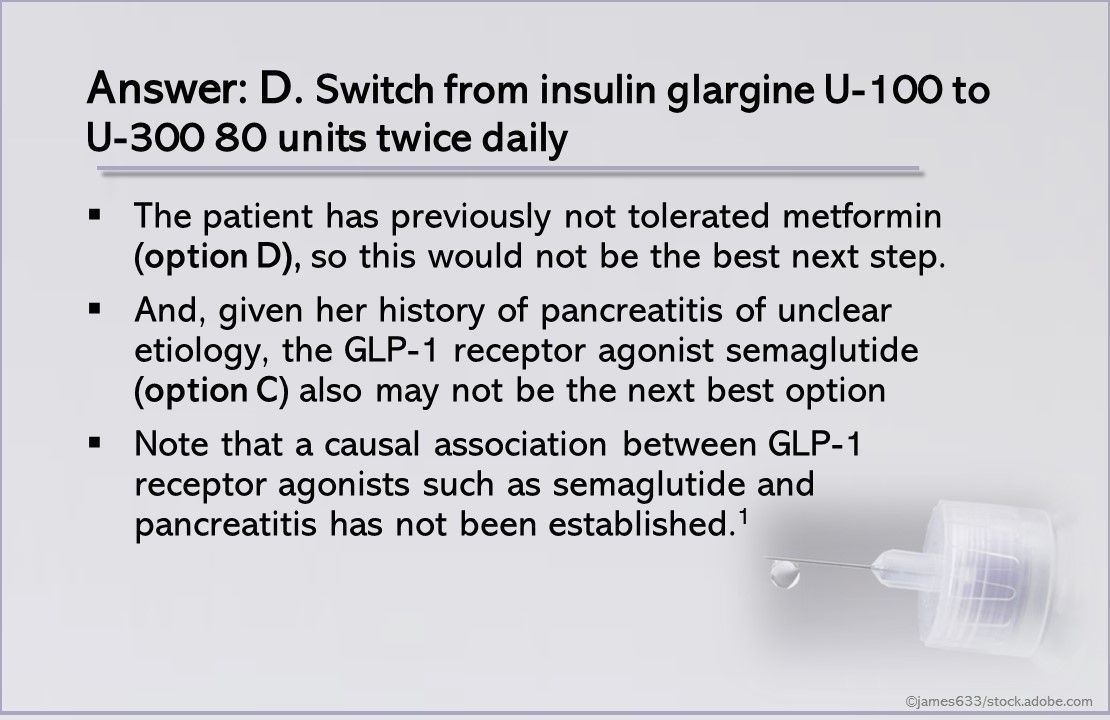
Given her history of pancreatitis of unclear etiology, semaglutide (option C) also may not be the next best option, although a causal association between GLP-1 receptor agonists such as semaglutide and pancreatitis has not been established.1
1. Das SR, Everett BM, Birtcher KK, et al. 2018 ACC Expert Consensus Decision Pathway on Novel Therapies for Cardiovascular Risk Reduction in Patients With Type 2 Diabetes and Atherosclerotic Cardiovascular Disease: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2018;72:3200-3223.
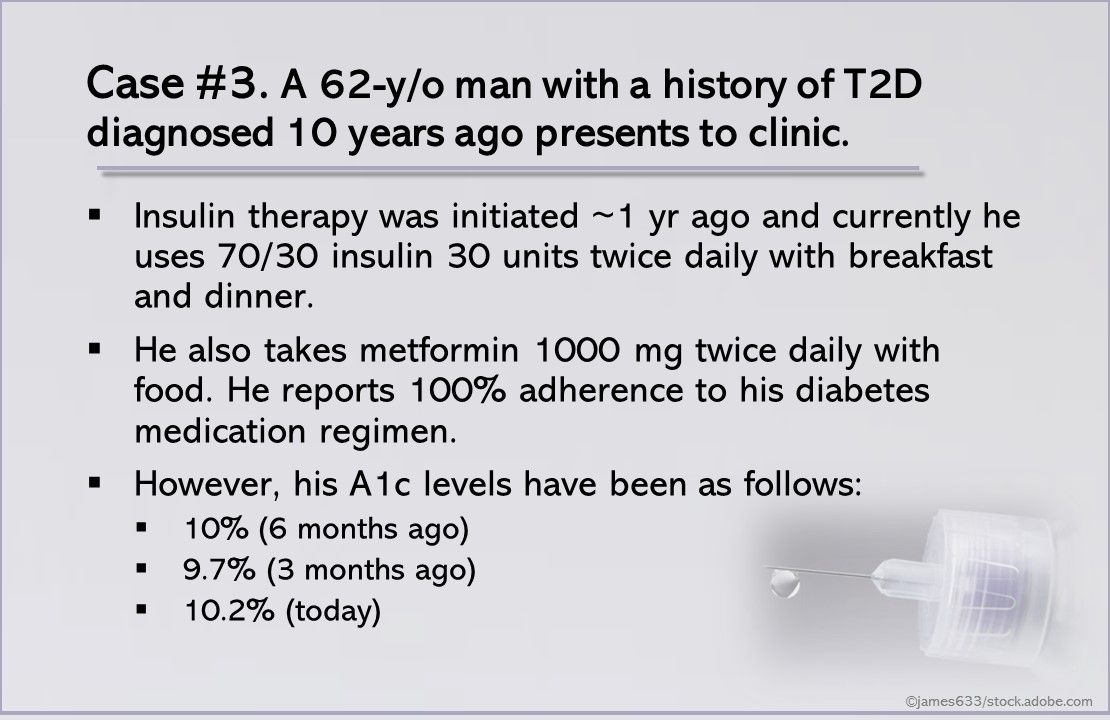
Case #3. A 62-y/o man with a history of T2D diagnosed 10 years ago presents to clinic. Insulin therapy was initiated about 1 year ago and currently he uses 70/30 insulin 30 units twice daily with breakfast and dinner. He also takes metformin 1000 mg twice daily with food. He reports 100% adherence to his diabetes medication regimen however his A1c level has trended back upward since his last appointment.






