© 2025 MJH Life Sciences™ , Patient Care Online – Primary Care News and Clinical Resources. All rights reserved.
Initiating Opioid Therapy for Chronic Pain: Does Which Medication Matter?
A new study compared opioid utilization trajectories of patients initiating tramadol, hydrocodone, and oxycodone. Key takeaways at-a-glance, here.
Although questions remain about the efficacy of opioid analgesics for the management of chronic pain, they are still frequently prescribed. The 3 most commonly prescribed opioids are short-acting/immediate release oxycodone, hydrocodone, and tramadol.
A recent study published in Pain Medicine sought to determine if there were any differences in patterns of use between these 3 medications over the year following initiation of therapy that might provide indications of efficacy and safety.
In the slides below, find key results and conclusions for clinicians.
Methodology. The retrospective study examined patterns of use of approximately 40 000 tramadol, 141 000 hydrocodone, and 45 000 oxycodone initiators. Patients were considered to have chronic pain if they were diagnosed with at least 1 of the following: back pain, neck pain, or osteoarthritis in the 90 days prior to index date when the opioid was first prescribed.
Study population. Over 70% of the patients had osteoarthritis and 35% had back pain. Participants with back pain were prescribed tramadol more frequently than oxycodone or hydrocodone.
Study purpose, participant groups. The study sought to determine the length of time the various medications were taken following initiation of therapy. For all the medications, 3 major groups were identified:
- Early discontinuers: Those who discontinued within first 5 weeks
- Late discontinuers: Those who discontinued between 5 weeks and
52 weeks - Persistent users: Those who were still taking the medications at
52 weeks
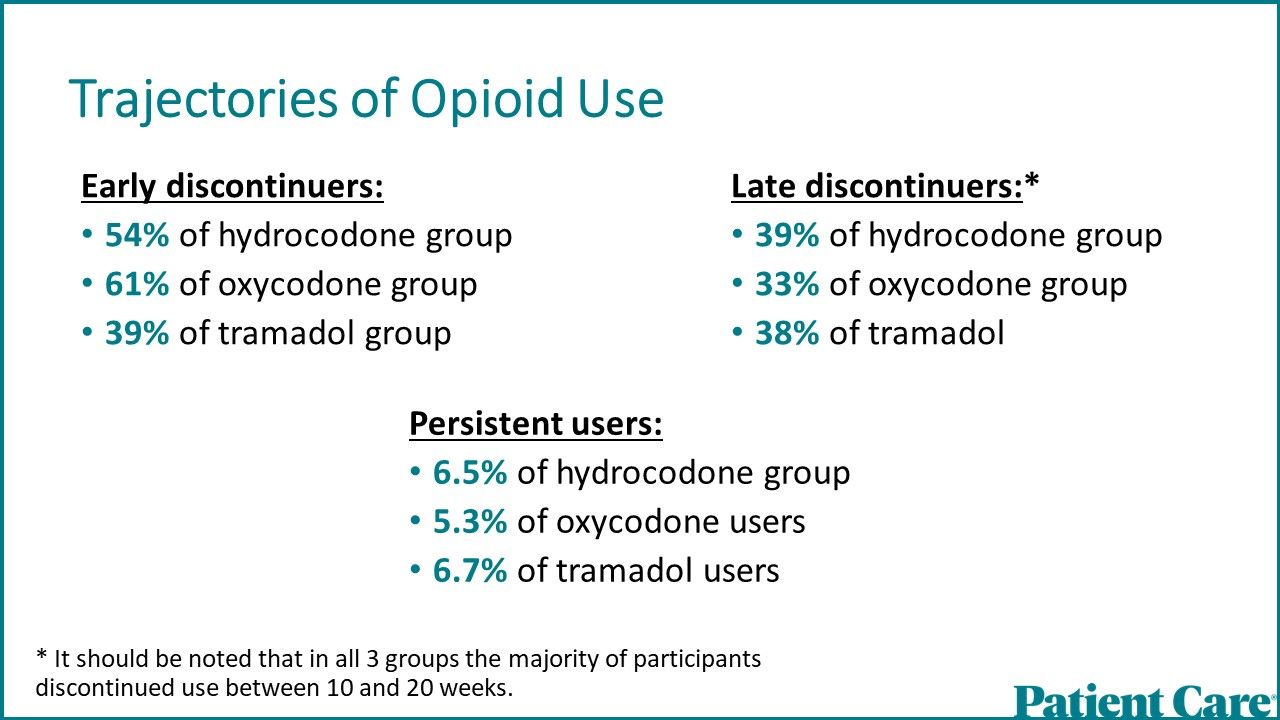
Trajectories of opioid use.
- Early discontinuers:
- 54% of hydrocodone group
- 61% of oxycodone group
- 39% of tramadol group
- Late discontinuers:*
- 39% of hydrocodone group
- 33% of oxycodone group
- 38% of tramadol users
- Persistent users:
- 6.5% of hydrocodone group
- 5.3% of oxycodone users
- 6.7% of tramadol users
*It should be noted that in all 3 groups the majority of participants discontinued use between 10 and 20 weeks.
Trajectories of use: Tramadol. For tramadol users an additional group was identified: intermittent users (16.4%) who after therapy was initiated decreased their use of the medication within the first 10 weeks of use but then continued use for the rest of the 52 weeks.
A rapid discontinuation trajectory was observed for 54% of hydrocodone and 61% of oxycodone users but for only 39% of tramadol users.
Factors linked with persistent use. Any surgery during the 6-month period prior to the index date was associated with a lower risk of persistent use of hydrocodone and oxycodone but did not affect the risk for tramadol. In contrast, the use of a skeletal muscle relaxant during the baseline period was associated with a lower risk of persistent use among tramadol users but was associated with a higher risk of persistent use among hydrocodone and oxycodone users.
Higher initial supply raises likelihood of persistent use. In all 3 medication groups it was found that the greater the initial days’ supply prescribed, the greater the likelihood of persistent use. Persistent use of all 3 medications was also associated with older age, Medicaid, more comorbidities, benzodiazepine use, gabapentinoid use, and antidepressant use.
Oxycodone users more likely to receive long-acting form. Oxycodone users were more likely to be prescribed long-acting opioids over the course of the year than were either hydrocodone or tramadol users. This may indicate that over time oxycodone users found less benefit from the short-acting form. Among persistent medication users, oxycodone users utilized a higher average weekly dose of medication than the tramadol or
hydrocodone users.
Conclusions. Study authors suggested that based on the requirement for higher doses of and more use of a long-acting form of oxycodone among those prescribed this medication, that it would appear to be the least preferable of the 3 medications for physicians to prescribe.
It should be noted that the study data were collected from 2008-2018, during which long-acting oxycodone was prescribed far more often than long-acting tramadol or long-acting hydrocodone (the latter not available until late in the study period), so the finding that the long-acting oxycodone was often prescribed may reflect a study artifact rather than a true difference between the medications.
Conclusions: Use of SNRIs may be beneficial. Although tramadol is often presented as a “safer” opioid due to its lower DEA classification as compared to hydrocodone and oxycodone, it appears that the likelihood of its persistent use is no less than for the 2 other medications. The intermittent trajectory seen with tramadol may reflect the drug’s specific composition. Tramadol combines an opioid with SNRI, and it is this latter action that appears to provide most of the medication’s analgesia. These results suggest that utilizing a SNRI—such as a tricyclic antidepressant, venlafaxine, or duloxetine—might be as beneficial as oxycodone and hydrocodone for this study population without the risks of abuse and addiction associated with the use of opioids.
Conclusions: Higher pain levels may drive persistent use. Some of the factors predictive of persistent use of the medications may reflect a continuing higher level of pain, including more comorbidities and older patients and concomitant use of antidepressants and gabapentinoids.
Conclusions: Concomitant use of opioids, benzodiazepines concerning. Other factors may reflect deficiencies in the care of patients with pain:
- Patients with Medicaid may be less likely to be offered non-medication therapies.
- The association of opioids with the use of benzodiazepines is concerning as benzodiazepines can reduce the analgesic effects of opioids, potentially leading to decreased pain relief when both classes of medications are prescribed together.
Reference: Acharya M, Hayes CJ, Li C, Painter JT, Dayer L, Martin BC. Opioid therapy trajectories of patients with chronic non-cancer pain over 1 year of follow-up after initiation of short-acting opioid formulations. Pain Med. 2024;25:173-186. doi:10.1093/pm/pnad169
Related Content:




