© 2025 MJH Life Sciences™ , Patient Care Online – Primary Care News and Clinical Resources. All rights reserved.
Imaging for Headaches: When is it Appropriate and Which Should be Employed?
Which initial imaging procedures are appropriate for different types of headache? Find out in our quick slideshow on the recently released guidelines from the American College of Radiology.
Headaches (HA) are among the most common reasons for which patients see physicians. Patients frequently fear that HA represents a serious, possibly fatal condition. Fortunately, this a rare scenario and most are primary HA for which there is no identifiable underlying etiology and no imaging studies are required.The American College of Radiology (ACR) recently issued a guideline on criteria for initial imaging of patients with HA associated with 7 clinical features. Click through the slides below for a compact review of when to use imaging and which type for assessment of HA associated with: severe and sudden onset, optic disc edema, “red flags,” migraine or tension-type, trigeminal autonomic origin, and chronic headaches with and without new or progressive features.
Most presenting HA are primary without dangerous underlying etiology and no imaging studies are required. However, physicians are appropriately concerned about missing those relatively rare cases where there is a serious underlying etiology that needs to be addressed-often quickly and sometimes on an emergency basis. Thus, they seek the balance between providing appropriate imaging for patients who require it while not over-testing. Overuse of imaging not only has financial implications but also, because radiation is involved in some studies, may be potentially harmful to patients.
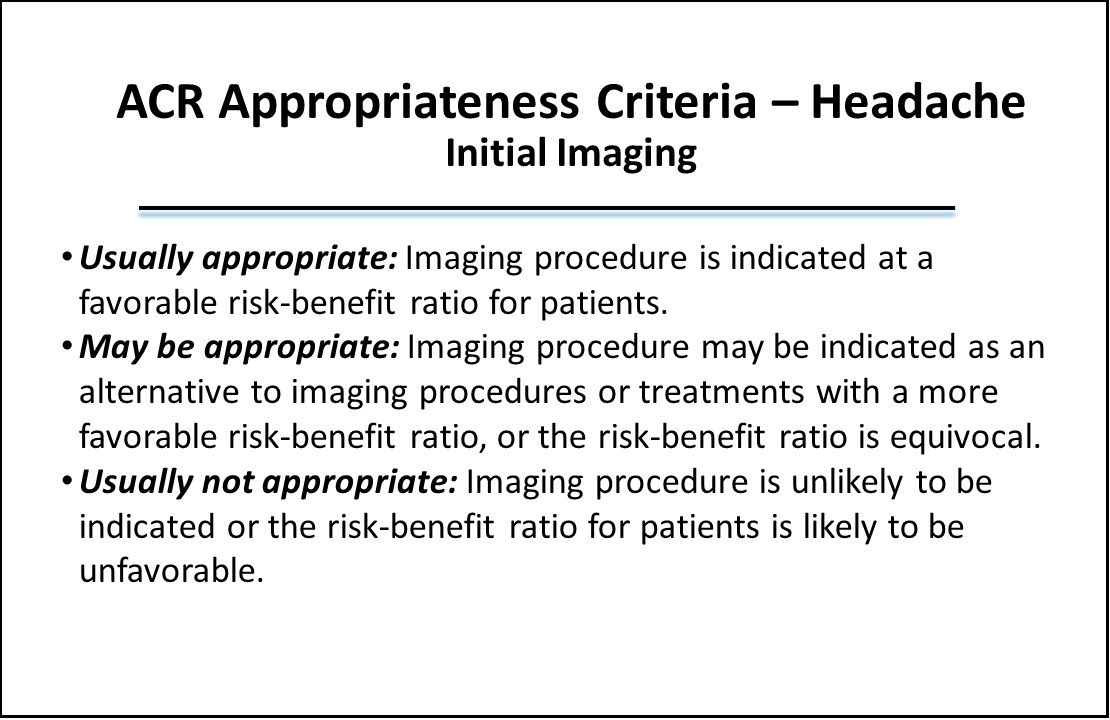
For each type of HA the ACR assessed which imaging procedures were deemed to be “Usually appropriate,” “May be appropriate,” and “Usually not appropriate,” as an initial test, as defined above. The slides that follow review only the common types of HA for which the guideline offers “Usually” or “May be” appropriate recommendations.
The guideline also includes a recommendation category where the studies may be appropriate but for which opinion among panel members varied to such an extent that only a recommendation of “may be appropriate (disagreement)” could be issued. That affects one type of study for one type of headache. Also included in the ACR guideline for each HA type but not included in this slide summary are imaging studies that ACR considers not to be usually appropriate.
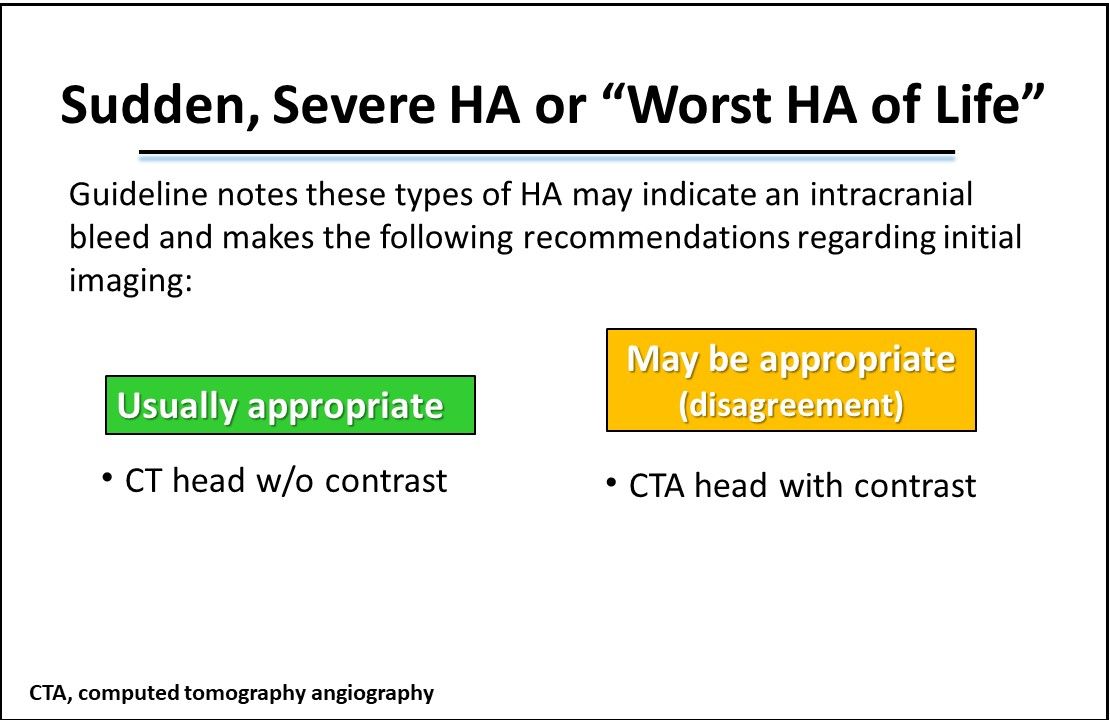
Sudden, Severe HA or “Worst HA of Life." The guideline notes these type of HA may indicate an intracranial bleed and makes the following recommendations regarding initial imaging:
- Head CT without contrast is the most appropriate initial imaging test.
- For Head CTA with IV contrast, there was disagreement as to whether it is usually appropriate. The guideline acknowledges that some patients may benefit from the test but there was disagreement over whether it should be considered an initial test, initial testing being the focus of the guidelines.
- No other imaging for initial assessment was considered to be indicated based on the current literature.
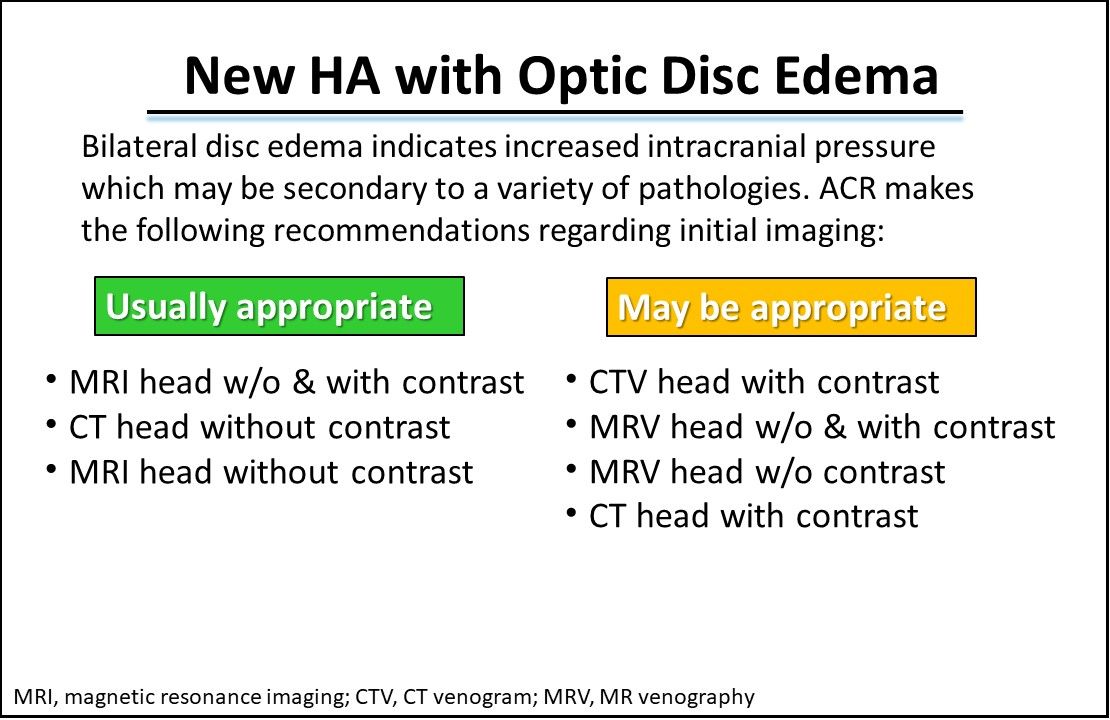
New HA with Optic Disc Edema. The guideline notes that bilateral disc edema indicates a rise in intracranial pressure which may be secondary to a variety of pathologies including tumors, hematoma, cerebral edema, and medications and makes the following recommendations regarding initial imaging:
- Usually appropriate: MRI head without and with IV contrast, CT head without contrast, MRI head without contrast
- May be appropriate: CTV head with contrast, MRV head without and with contrast, MRV head without contrast, CT head with contrast
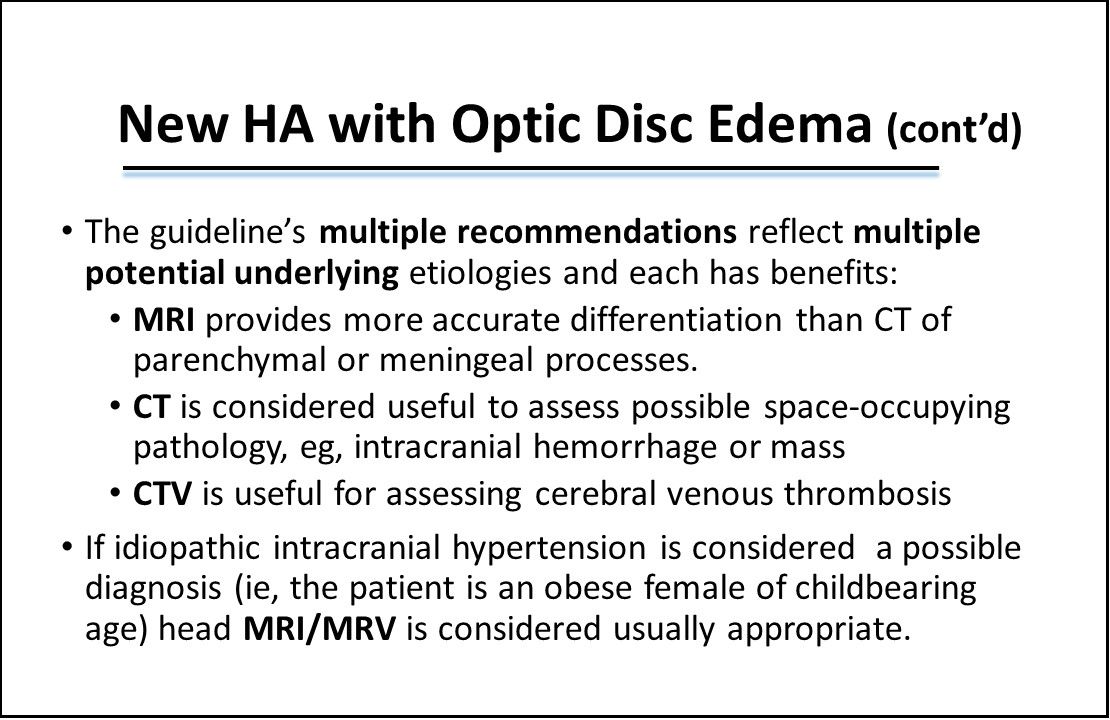
New HA with Optic Disc Edema (cont'd). The guideline’s multiple recommendations reflect multiple potential underlying etiologies and each has benefits:
- MRI provides more accurate differentiation than CT of parenchymal or meningeal processes.
- CT is considered useful to assess possible space-occupying pathology, eg, intracranial hemorrhage or mass.
- CTV is useful for assessing cerebral venous thrombosis.
Also, if idiopathic intracranial hypertension is considered a possible diagnosis (ie, the patient is an obese female of childbearing age) head MRI/MRV is considered usually appropriate.
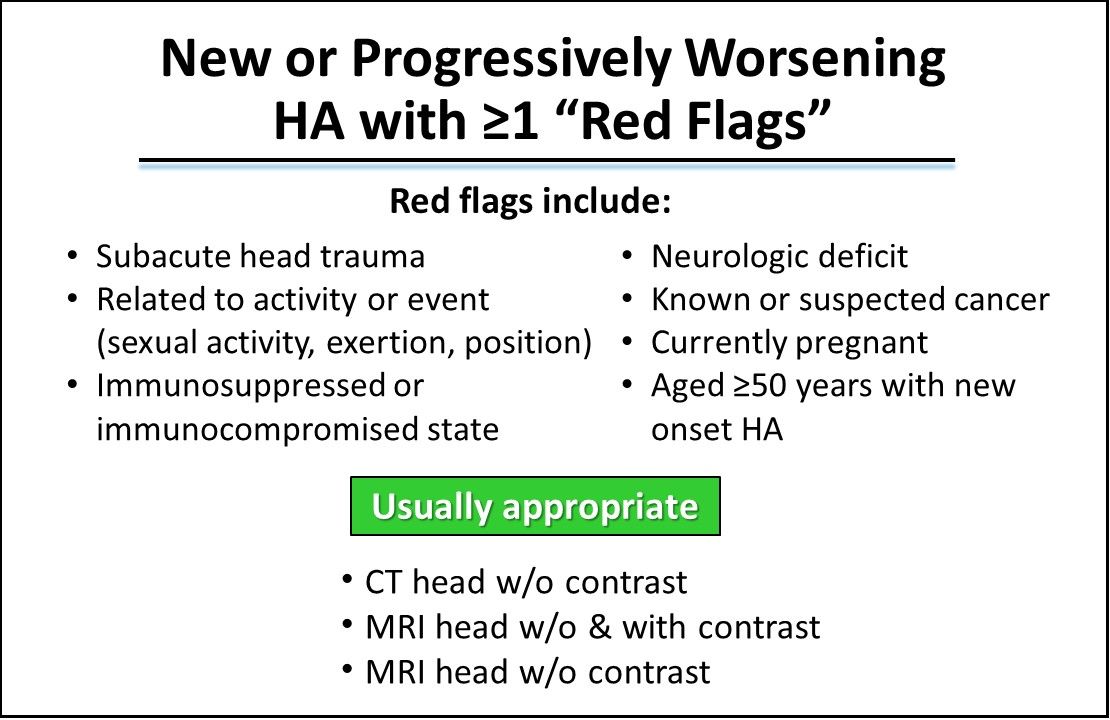
New or Progressively Worsening HA with ≥1 “Red Flags." The red flags include head trauma, cancer, immunocompromised state, pregnancy, patients 50 years or older with new onset HA, related to activity or position, or with a corresponding neurologic deficit. The imaging procedures that the ACR deemed usually appropriate for this type of HA were CT head without contrast, MRI head without and with contrast, and MRI head without contrast.
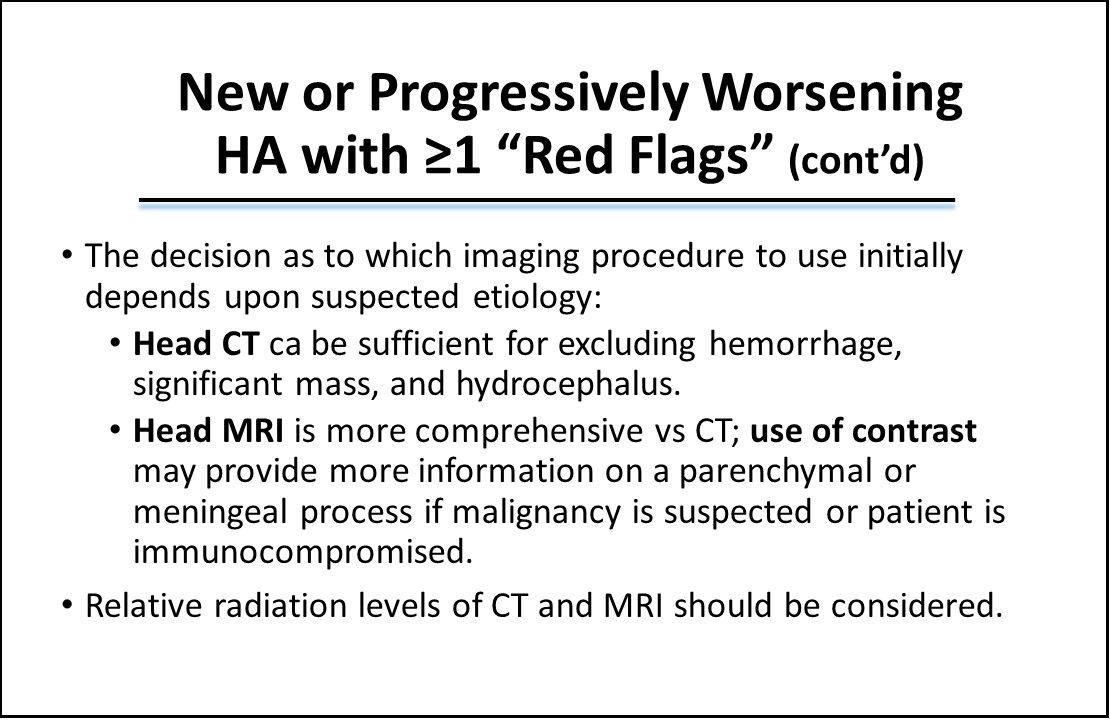
New or Progressively Worsening HA with ≥1 “Red Flags” (cont’d). The decision as to which imaging procedure to use initially depends upon suspected etiology:
- Head CT sufficient for excluding hemorrhage, significant mass, and hydrocephalus.
- Head MRI is more comprehensive vs CT; use of contrast may provide more information on a parenchymal or meningeal process if malignancy is suspected or patient is immunocompromised.
- Relative radiation levels of CT and MRI should be considered.
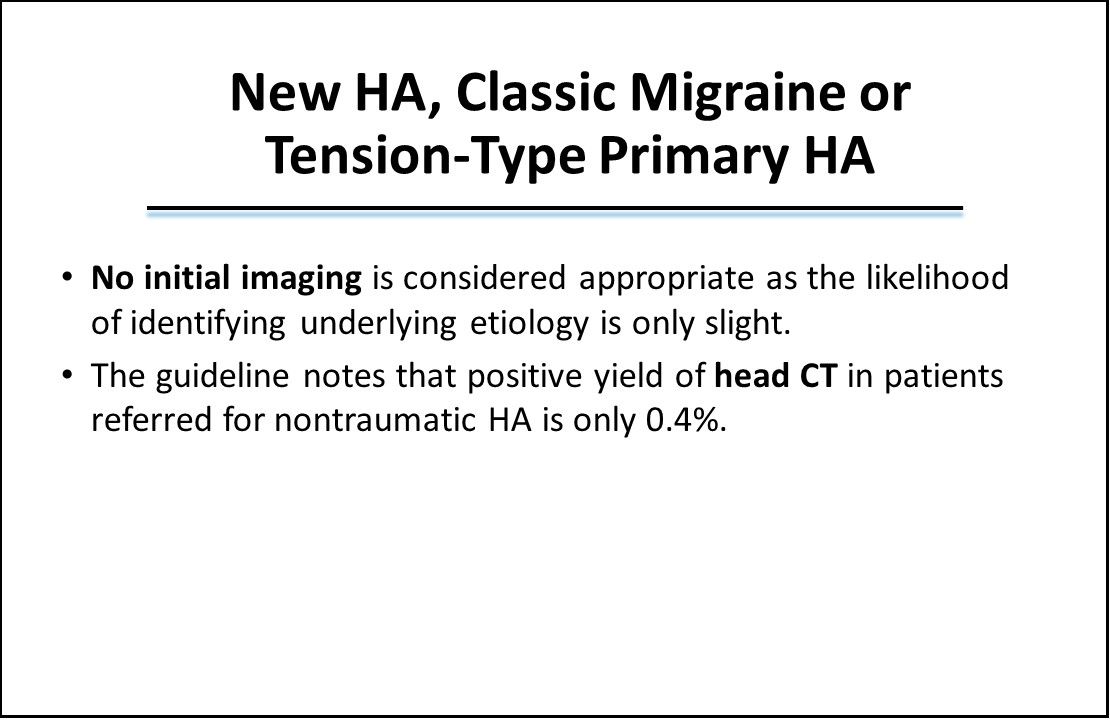
New HA, Classic Migraine or Tension-Type Primary HA. No initial imaging was considered appropriate as the likelihood of identifying underlying etiology is only slight. The guideline did note that positive yield of head CT in patients referred for nontraumatic HA is only 0.4%.
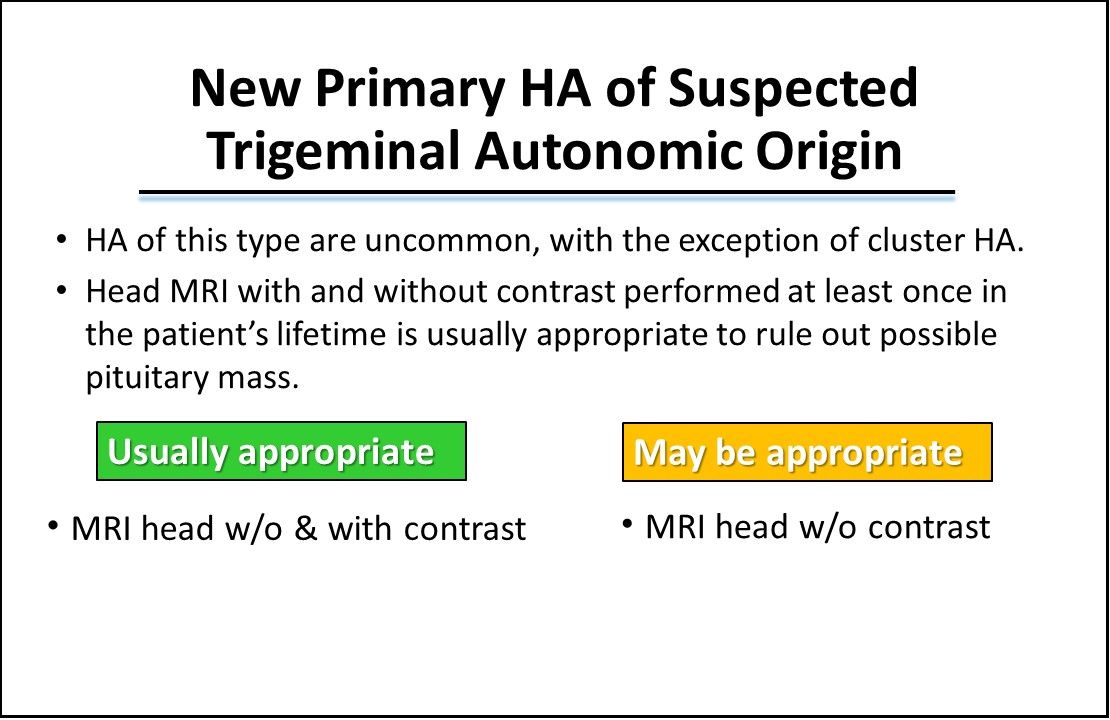
New Primary HA of Suspected Trigeminal Autonomic Origin. The guideline notes that with the exception of cluster HA, these types of HA are uncommon. Head MRI with and without contrast performed at least once in the patient’s lifetime is usually appropriate to rule out possible pituitary mass. The guideline recommends that MRI head without and with contrast is usually appropriate and MRI head without contrast may be appropriate.
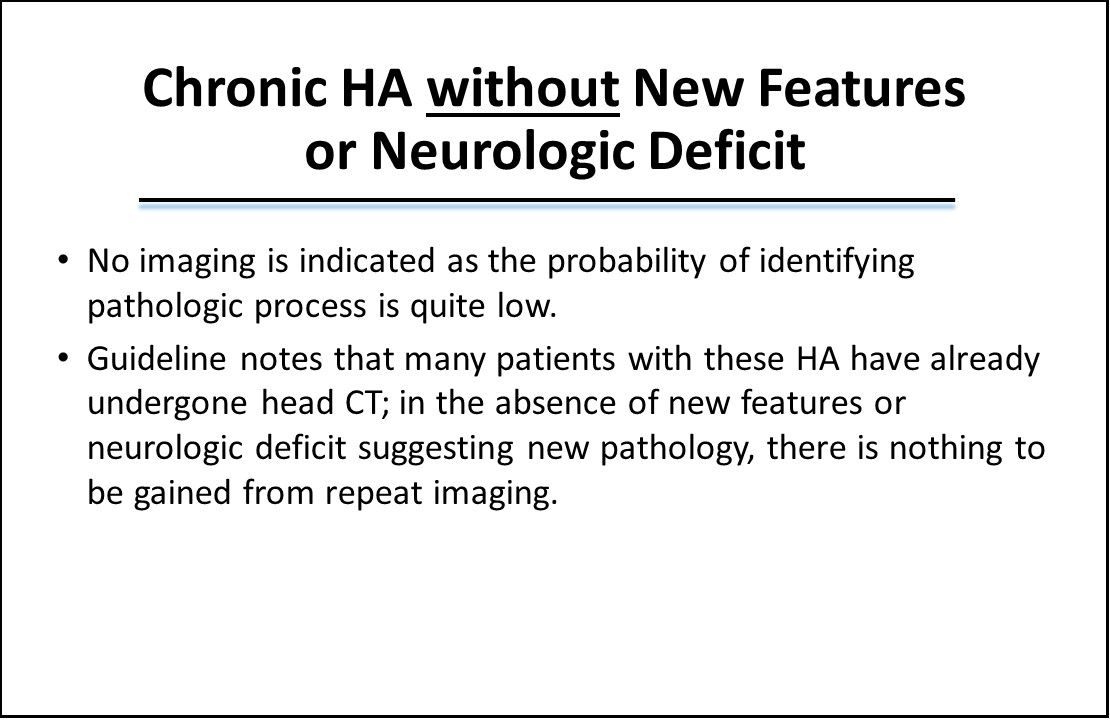
Chronic HA without New Features or Neurologic Deficit. No imaging is indicated as the probability of identifying pathologic process is quite low. The guideline notes that many patients with these HA have already undergone head CT and in the absence of new features or neurologic deficit suggesting new pathology, there is nothing to be gained from repeat imaging.
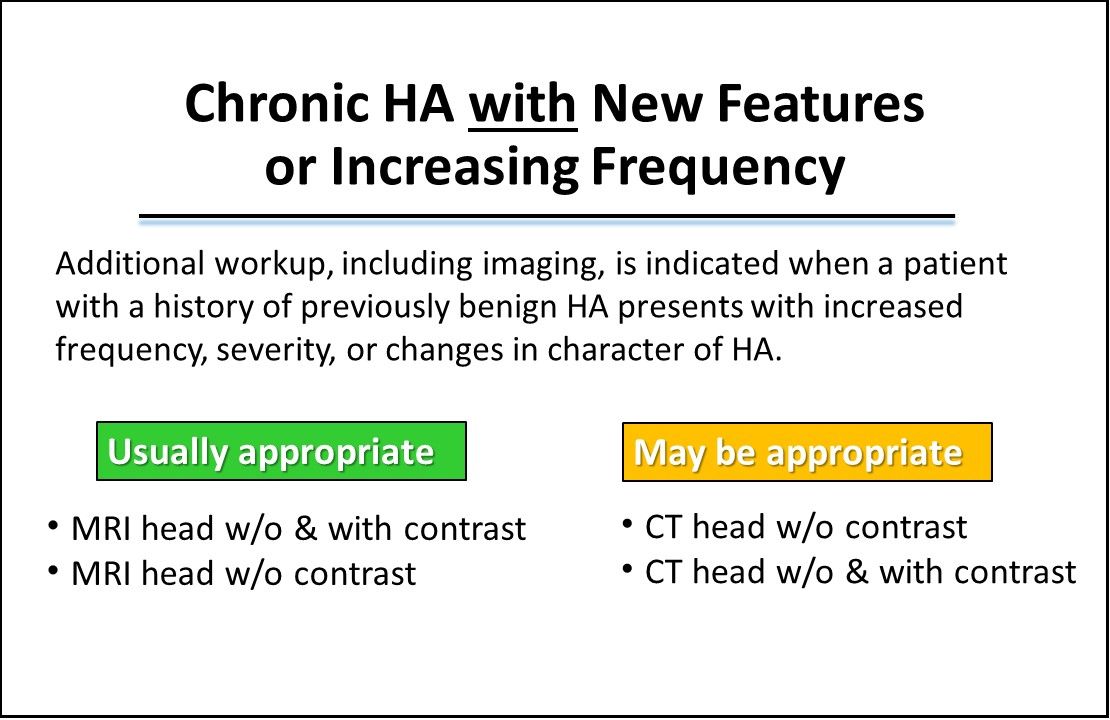
Chronic HA with New Features or Increasing Frequency. Additional workup, including imaging, is indicated when a patient with a history of previously benign HA presents with increased frequency, severity, or changes in character of HA. The guideline indicated that MRI head without and with contrast as well as head MRI without contrast are usually appropriate imaging procedures for this HA type. Also, CT head without contrast along with CT head without and with contrast may be appropriate imaging procedures.
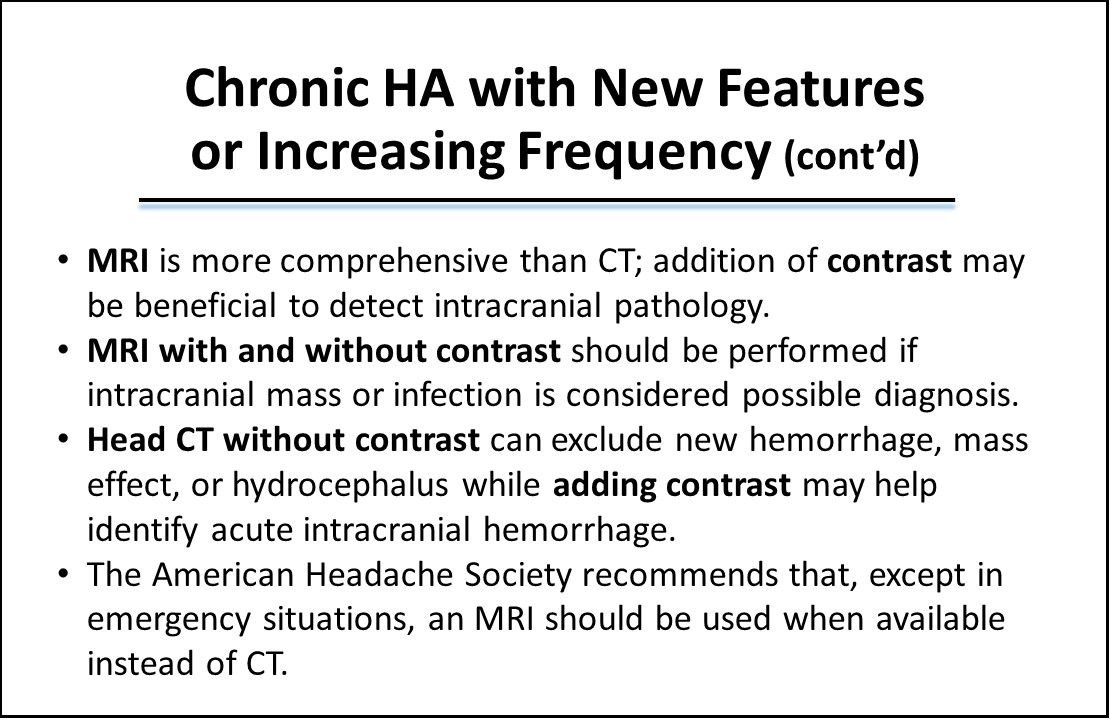
Chronic HA with New Features or Increasing Frequency (cont’d).
- MRI is more comprehensive than CT; addition of contrast may be beneficial to detect intracranial pathology.
- MRI with and without contrast should be performed if intracranial mass or infection is considered possible diagnosis.
- Head CT without contrast can exclude new hemorrhage, mass effect, or hydrocephalus while adding contrast may help identify acute intracranial hemorrhage.
- American Headache Society recommends that, except in emergency situations, an MRI should be used when available instead of CT.
The Issue of Radiation Exposure.
- For each of imaging procedures the guideline reviewed, it provides the relative radiation levels.
- Important to remember that when considering MRI vs CT in a situation where both are indicated as “usually appropriate” for a specific type of HA, that MRI is not associated with any significant radiation exposure while CT is.
- The issue of radiation exposure is especially important for the pediatric age group and for pregnant women.
Reference: Expert Panel on Neurologic Imaging, Whitehead MT, Cardenas AM, et al. ACR Appropriateness Criteria® Headache. J Am Coll Radiol. 2019;16:S364-S377.
Stay in touch with Patient Care® Online:
→Subscribe to ourNewsletter →Like us on Facebook →Follow us on Twitter →Write or Blog for Patient Care® Online→Follow us on LinkedIn
