© 2025 MJH Life Sciences™ , Patient Care Online – Primary Care News and Clinical Resources. All rights reserved.
How to Manage COPD Exacerbations: A Few FAQs
Pulmonologist Jonathan Ilowite, MD, answers 5 of the many common questions he fields about COPD exacerbations and how to manage them.
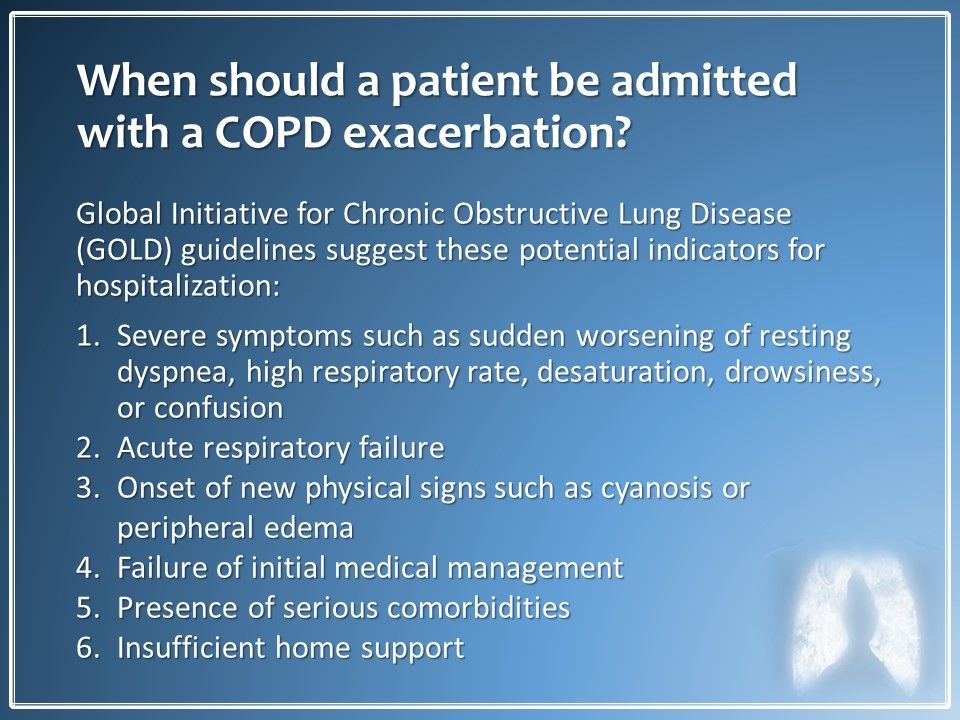
When should a patient be admitted for a COPD exacerbation? The GOLD guideline criteria for hospital admission for a COPD exacerbation are mostly subjective. My personal approach if a patient is not well-controlled on outpatient therapy or I see the patient in the emergency department and he/she still does not look well after initial treatment, it is time for admission.
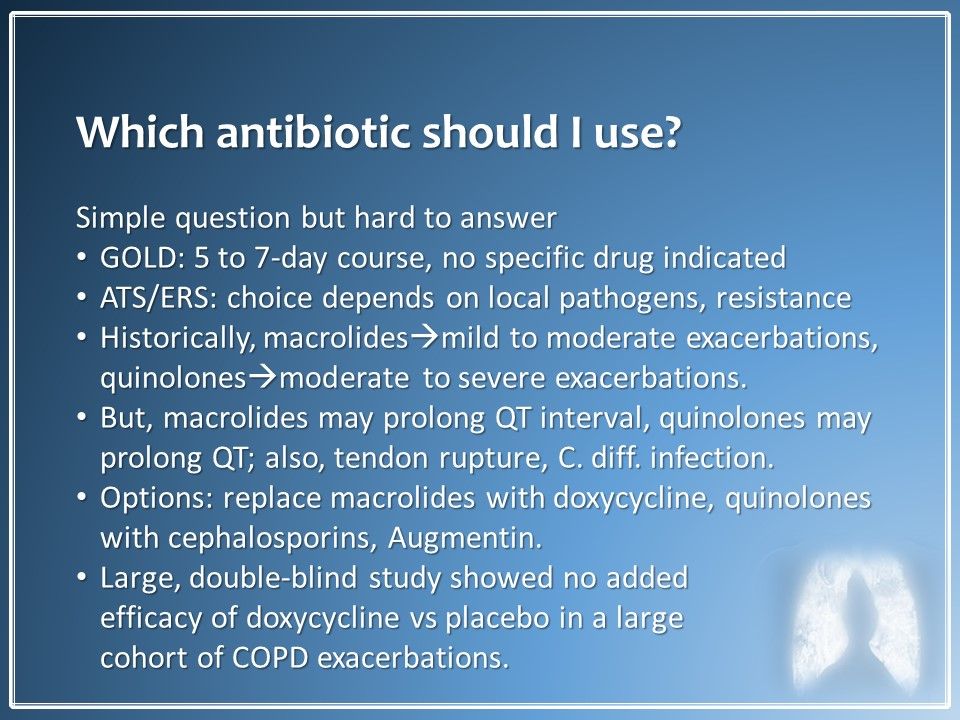
Which antibiotics should I use to treat a COPD exacerbation? It seems like a simple question but the answer is not straightforward. Guidelines from GOLD and from the American Thoracic Society/European Respiratory Society are not particularly prescriptive. I have favored the macrolides and quinolones for the past 10 years but they have had their problems. The evidence for doxycycline for COPD exacerbations is lacking, in my opinion. I will use quinolones if I suspect Pseudomnas infection and use macrolides for milder outpatient exacerbations.
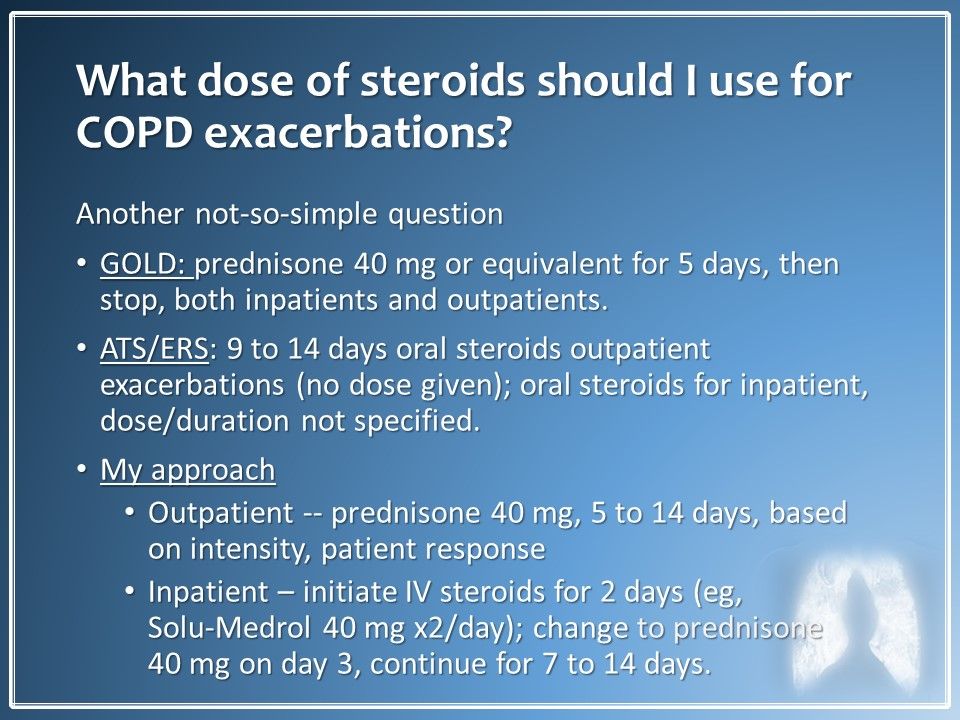
What dose of steriods should I use for a COPD exacerbation? Another answer that is not straightforward. The GOLD guideline recommendation for prednisone or equivalent is a strong one. ATS/ERS guidelines leave open decisions on outpatient dosing and on inpatient dosing and duration of steroid treatment. I have been reducing both the amount and duration of steroids I use since recent literature comparing higher dose or duration treatment to lower has shown no differences. Unless I plan on continuing steroids for more than 2 weeks, I no longer taper them.
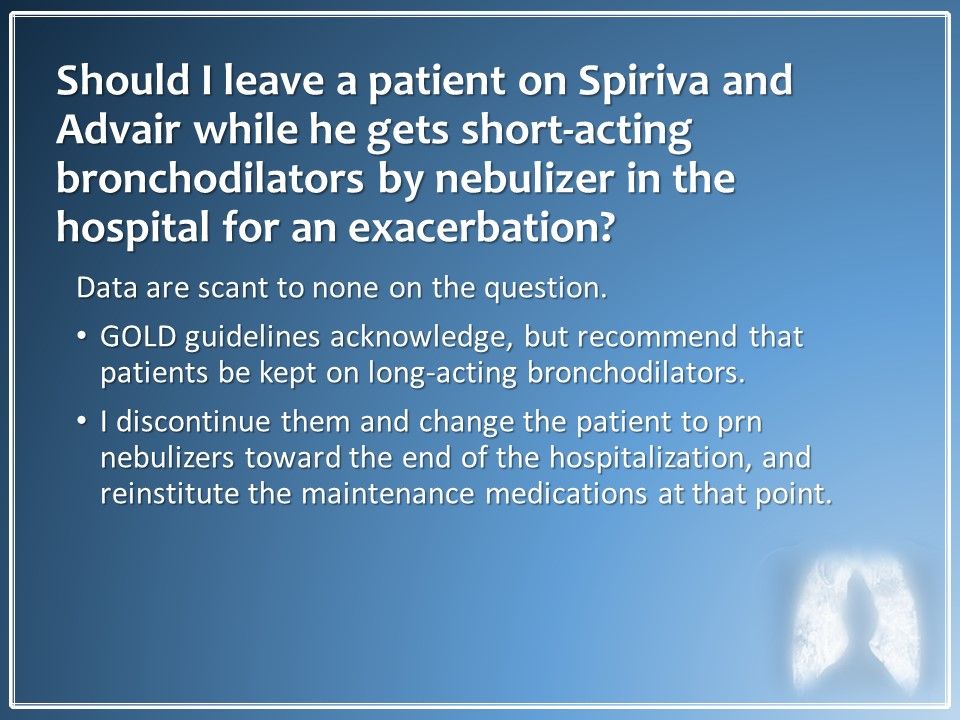
Should I leave a patient on Spiriva and Advair during nebulized short-acting bronchodilator therapy in the hospital? GOLD guidelines recommend that patients remain on their long-acting bronchodilators. I discontinue the outpatient drugs on admission and then shift to prn nebulizers as discharge approaches followed by reinstitution of maintenance medications when the patient leaves.
Should I use noninvasive ventilation (NIV) for COPD exacerbations? The answer to this is absolutely, yes. Note that in pivotal studies of NIV there was wide variability in NIV devices, in the settings for and duration of therapy so it is hard to be specific on recommendations.
How can I prevent patient readmission to the hospital within 30 days? This is the 1 million dollar question and hospitals are under significant financial pressure to avoid these readmissions 30 days after discharge. The tactics above were formulated by an emergency task force I headed up at my institution.
Results of our efforts. The good news is that the average length of stay for after an admission for COPD exacerbation was reduced--and even without a monetary value attached to that or a specific 30-day readmission metric, a needle was moved.
If these are questions you ask or have asked, I hope the answers here are useful.
Please check out the guildelines below.
Global Initiative for Chronic Obstructive Lung Disease. Gold Guidelines. www.goldcopd.org Accessed December 4, 2018.
Wedzicha JA, Miravitlles M, Hurst JR, et al. Management of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J. 2017;49(3).
In this short slide show, I will summarize my responses to some common questions I hear, sometimes from colleagues, sometimes from students, on the topic of COPD exacerbations. I will provide a topline answer drawn from current clinical practice guidelines and follow that with my own personal approaches and biases as well. Â




