© 2025 MJH Life Sciences™ , Patient Care Online – Primary Care News and Clinical Resources. All rights reserved.
Emesis x3 Weeks in an Elderly Woman: Dx?
ECG Challenge: The patient is seen in the ED after a short-lived reprieve from vomiting. She faints during the ECG. What’s your read of the tracing?
Click through the patient's brief presenting history, review the ECG, and see if your impressions are correct.
Patient history: An elderly woman comes to the ED because she has been vomiting for 3 weeks. She was already hospitalized for this and no definite cause was determined. She improved and was discharged yesterday, but the vomiting is now just as bad again, even though she has been taking ondansetron at home.
Vital signs and examination. Her vital signs are normal except for mild tachycardia. The physical exam is otherwise normal except for mucous membranes that appear a bit dry. Initial thoughts on differential include: Bowel obstruction, marijuana hyperemesis, medication side effect, viral syndrome.
Initial testing. Blood work, ECG, abdominal x-ray are ordered. Just before the patient is taken to the x-ray department, the ECG tech comes in with the ECG tracing (next slide) and says the patient fainted during the ECG and that the nurse did a precordial thump.
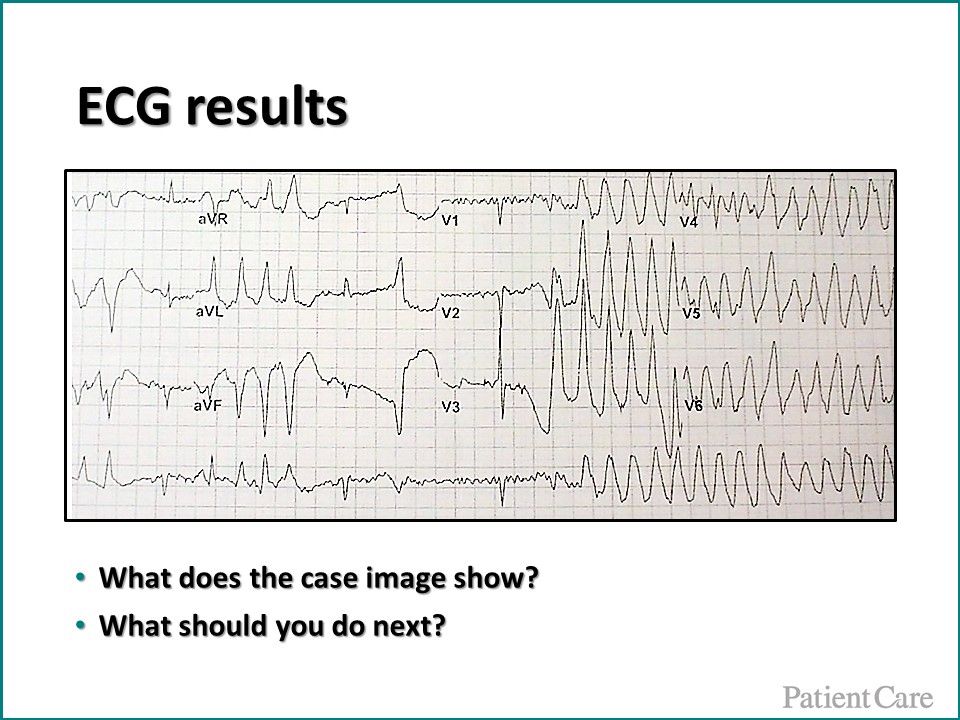
ECG results. The ECG tracing is shown above. When you walk into the room the patient is awake. What does the ECG show? What should you do next?
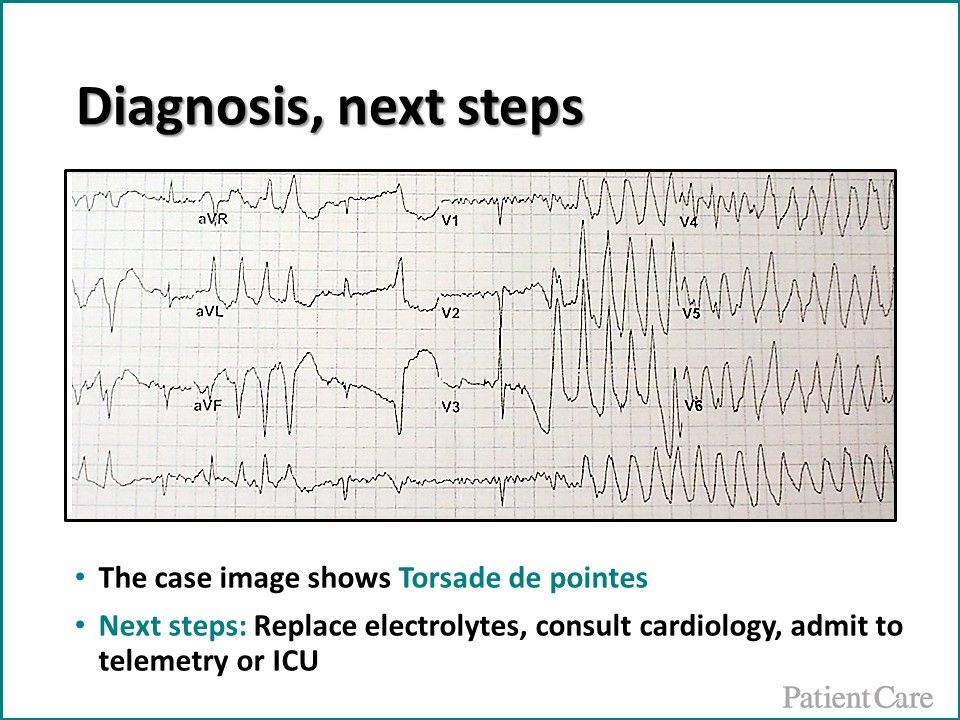
Diagnosis, next steps. The diagnosis is Torsade de pointes. The patient needs electrolyte replacement, admission to telemetry or ICU and you also call an immedite cardiology consult.
Torsade de pointes. Often shortened to "Torsade," the arrhythmia is a form of polymorphic ventricular tachycardia that is often transient, but may be fatal. It is often caused by medical conditions or medications that prolong the QT interval. Low levels of potassium, calcium, and magnesium may all contribute. Additional risk factors include age, female gender, bradycardia, and CHF.
Torsade treatment. Treatment is typically with empiric magnesium and defibrillation if necessary. If antiarrhythmics are tried, only lidocaine or phenytoin (vs amioadarone, procainamide) should be used as neither prolongs QT interval. To prevent recurrence, discontinue or avoid medications that may prolong QT interval and replace electrolyes; bradycardia may also need to be more aggressively treated than is routine.
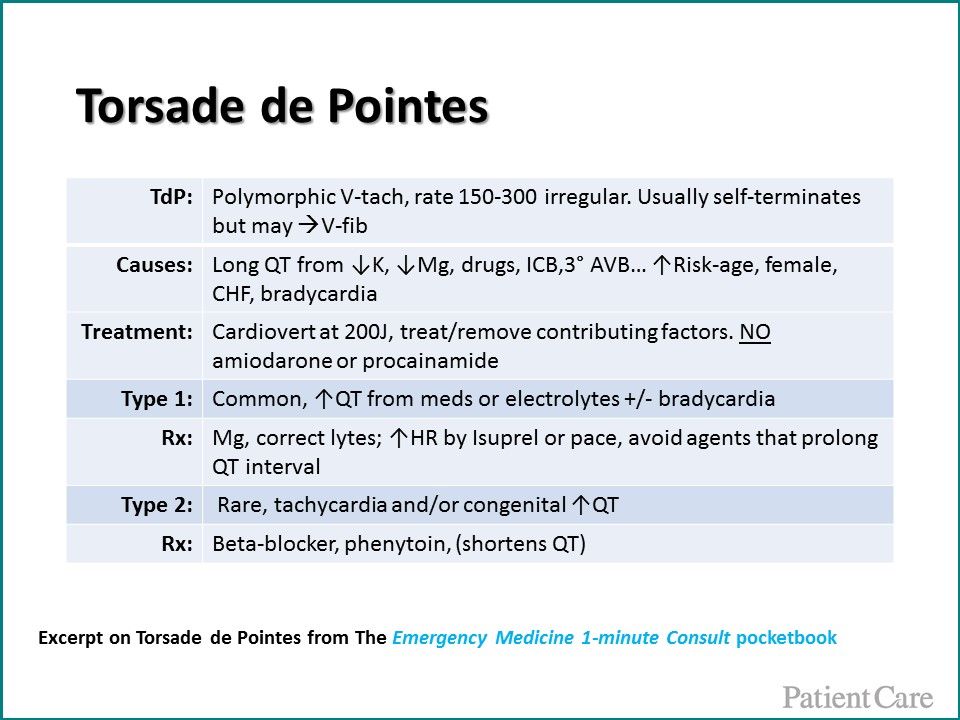
Torsade de Pointes, at-a-glance, from The Emergency Medicine 1-minute Consult pocketbook.




