© 2025 MJH Life Sciences™ , Patient Care Online – Primary Care News and Clinical Resources. All rights reserved.
Cardiology Update: 6 New Things From ACP
It’s time to rethink aspirin; there’s optimism about the PCSK9 inhibitors; and new help for people with valvular heart disease. What else is new in cardiology?
At the American College of Physicians Internal Medicine Meeting 2015 in Boston, Peter Zimetbaum, MD, Associate Professor of Medicine, Harvard Medical School, presented an “Update In Cardiology.” Here are the highlights of his presentation and the implications for clinical practice.
Definite uses for aspirin in primary prevention of CVD include: multiple risk factors for vascular disease (older age, hypertension, smoking, hyperlipidemia). Questionable indications for aspirin: moderate risk over 10 years. No indication: low-risk patients.
Preliminary evidence suggests a benefit on cardiovascular mortality with PCSK9 inhibitors. They induce about 60% reduction in LDL cholesterol that is durable for at least 52 weeks. Adverse events with PCSK9 inhibitors include injection site reactions and neurocognitive effects.
Use adjuncts to statin therapy in patients who cannot get to target lipid levels on statins alone and in statin-intolerant patients. Change in target LDL to lower values.
Aspirin is no longer recommended for thromboembolic prophylaxis. New oral anticoagulants are recommended equally with warfarin for thromboembolic prophylaxis. The Watchman⢠Left Atrial Appendage Closure Device is an alternative for thromboembolic prophylaxis in patients with contraindication to oral anticoagulants.
Two FDA-approved valves are now available for patients at high risk for complications from aortic valve surgery. Choice of the valves is based mostly on technical/anatomic considerations. The valves are capable of being placed within failing aortic valve prosthesis.
Newer generations of devices have smaller delivery systems and are technically easier to place and reposition. Major complications include vascular trauma, stroke, paravalvular aortic regurgitation, heart block. The long-term durability of these valves is still unknown.
Dual antiplatelet therapy (DAPT) provides some benefit up to 30 months. Weigh against an increased bleeding risk in patients with a drug-eluting stent (DES). If the risk of bleeding is minimal, there is likely an advantage to continued DAPT. Discontinue or interrupt DAPT after 6 months (perhaps even 3 months) if bleeding risk necessitates.
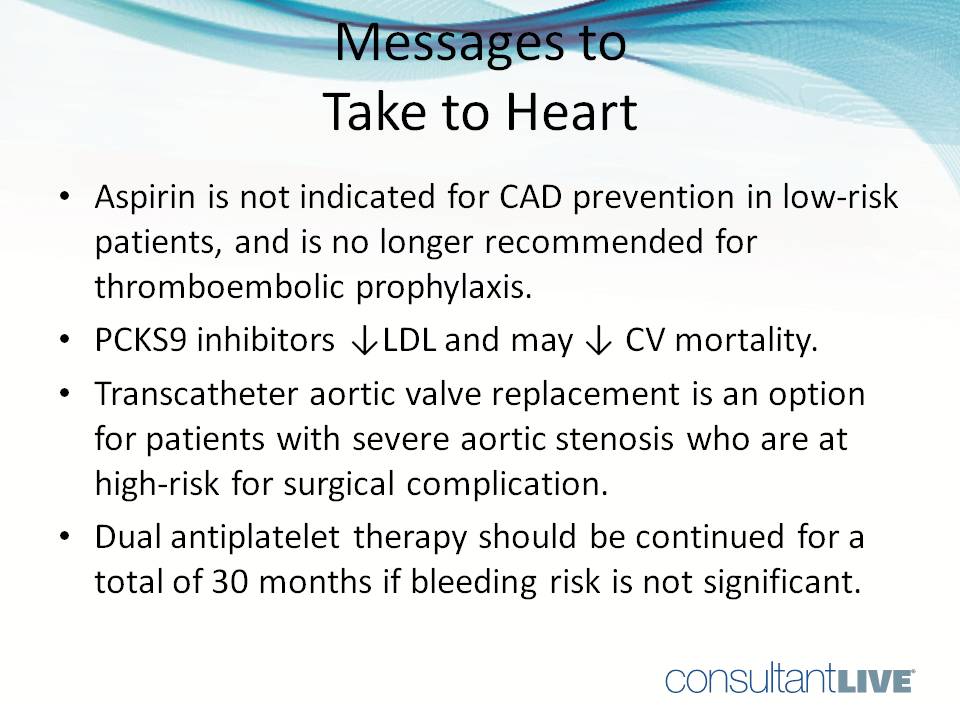
• Transcatheter aortic valve replacement is an option for patients with severe aortic stenosis and high risk for surgical complication.
• Aspirin is not indicated for CVD prevention in low-risk patients.
• Dual antiplatelet therapy should be continued for a total of 30 months if the bleeding risk is not significant.
• PCKS9 inhibitors are effective at lowering LDL and may reduce cardiovascular mortality.
• Aspirin is no longer recommended for thromboembolic prophylaxis
At the American College of Physicians Internal Medicine Meeting 2015 in Boston, Peter Zimetbaum, MD, Associate Professor of Medicine at Harvard Medical School, presented an “Update In Cardiology.”Here are the highlights of his presentation-and the implications for primary care clinical practice.
Related Content:



