© 2025 MJH Life Sciences™ , Patient Care Online – Primary Care News and Clinical Resources. All rights reserved.
After Metformin: Which Class Would you Choose?
In this older patient with T2DM, HFpEF, and other comorbidities, which class of medication is most appropriate--and guideline-recommended?
Mrs Anderson is in your office for T2DM follow-up. She is 69-years-old and is in your office for follow-up management of her type 2 diabetes (T2DM). You are about to choose an add-on antihyperglycemic medication for her. A recap of her visit is shown above.
ACC/AHA CVD Prevention Guideline recommendations. The 2019 ACA/AHA Guideline on Prevention of Cardiovascular Disease recommends a target of <130/80 mm Hg for those on pharmacologic therapy for hypertension, so the increase in lisinopril dose is appropriate. Also, in this patient with T2DM, hypertension, and microalbuminuria, strict BP targets are essential in order to prevent progression of her renal disease. Next, the ACC/AHA recommends (class 1) initiating at least a moderate-intensity statin in a patient with diabetes who is aged 40 to 75 years-with a recommendation for further risk assessment to consider a high-intensity statin.
Which diabetes medication to add her regimen? ACC/AHA primary CVD prevention guidelines recommend either a SGLT2 inhibitor or GLP-1 RA as second-line. Either class is reasonable for this patient -- but first clinicians should enter a shared decision making discussion to ensure risks/benefits are understood and to consider patient lifestyle factors that may affect medication choice.
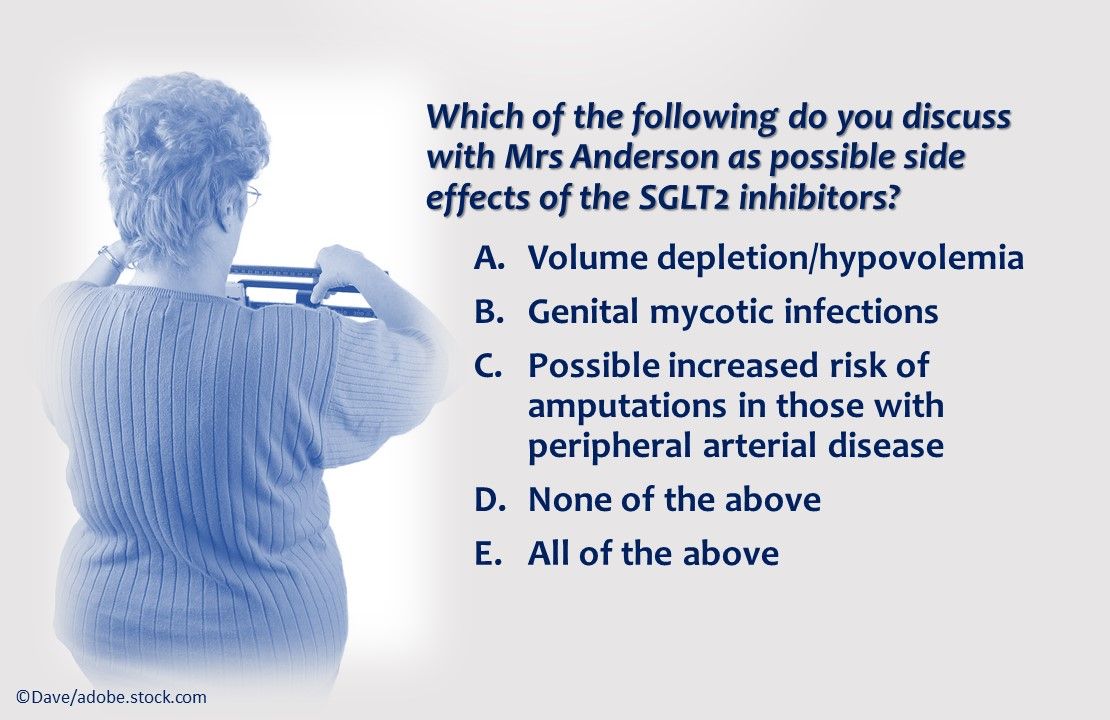
Which of the above do you discuss with Mrs Anderson as possible side effects of the SGLT2 inhibitors?
Answer: E. All of the above. Volume depletion/hypovolemia, genital mycotic infections, possible increased risk of amputations in those with peripheral arterial disease are all possible side effects of SGLT2 inhibitors. A signal for possible increased risk of amputations was noted with canagliflozin only (not thought to be a class effect).
Answer: A. Reduction in heart failure hospitalizations. All of the other positive outcomes are associated with GLP-1 RA therapy but there is no apparent class effect on heart failure.
During early post-marketing surveillance, increased signals were detected for pancreatitis or pancreatic cancer, but the FDA did not confirm the findings. A possible inreased risk of retinopathy, as seen with semaglutide in the SUSTAIN-6 trial, was noted but has not appeared consistently in the FDA adverse event database with other GLP-1 RAs. Routine eye exams are recommended for all patients with diabetes.
*semaglutide, liraglutide
Either a GLP-1 RA or SGLT2 inhibitor would be appropriate for Mrs Anderson. The former are delivered via injection while the latter are taken orally, daily; one option may be preferred based on lifestyle considerations. Given the demonstrated cardiovascular benefits of these antidiabetic drugs, the ACC released in 2018 its Expert Consensus Decision Pathway on Novel Therapies for CV Risk Reduction in Patients with Type 2 Diabetes and Atherosclerotic Cardiovascular Disease to guide not just cardiologists but all clinicians who treat patients with diabetes, in the management of patients with diabetes and concurrent heart disease or those at risk for heart disease.
For the case introducing Mrs Anderson, please click here: The "Sweet Spot" in Type 2 Diabetes Management
Additional resources
ACC Key perspectives
https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2019/03/07/16/00/2019-acc-aha-guideline-on-primary-prevention-gl-prevention
Prevention Guidelines made simple: selection of figures and tables
http://www.onlinejacc.org/sites/default/files/additional_assets/guidelines/Prevention-Guidelines-Made-Simple.pdf






