© 2025 MJH Life Sciences™ , Patient Care Online – Primary Care News and Clinical Resources. All rights reserved.
2022 CDC Guideline for Prescribing Opioids: A 10-question Quiz
Get up-to-date on the newest guidance for clinicians managing acute, subacute, and chronic pain in adults with this quick quiz.
The US Centers for Disease Control and Prevention (CDC) released new recommendations for clinicians on managing acute (duration of <1 month), subacute (1-3 months), and chronic (>3 months) pain in adults.
The new guidance replaces the CDC Guideline for Prescribing Opioids for Chronic Pain released in 2016, which was interpreted by the health care community as imposing strict opioid dose and duration limits and was misapplied by some organizations, bringing outcry from persons with chronic pain and their advocates and prompting guideline authors to clarify their recommendations in 2019.
Refresh your memory of the CDC Clinical Practice Guideline for Prescribing Opioids for Pain — United States, 2022 with the 10-question quiz below.
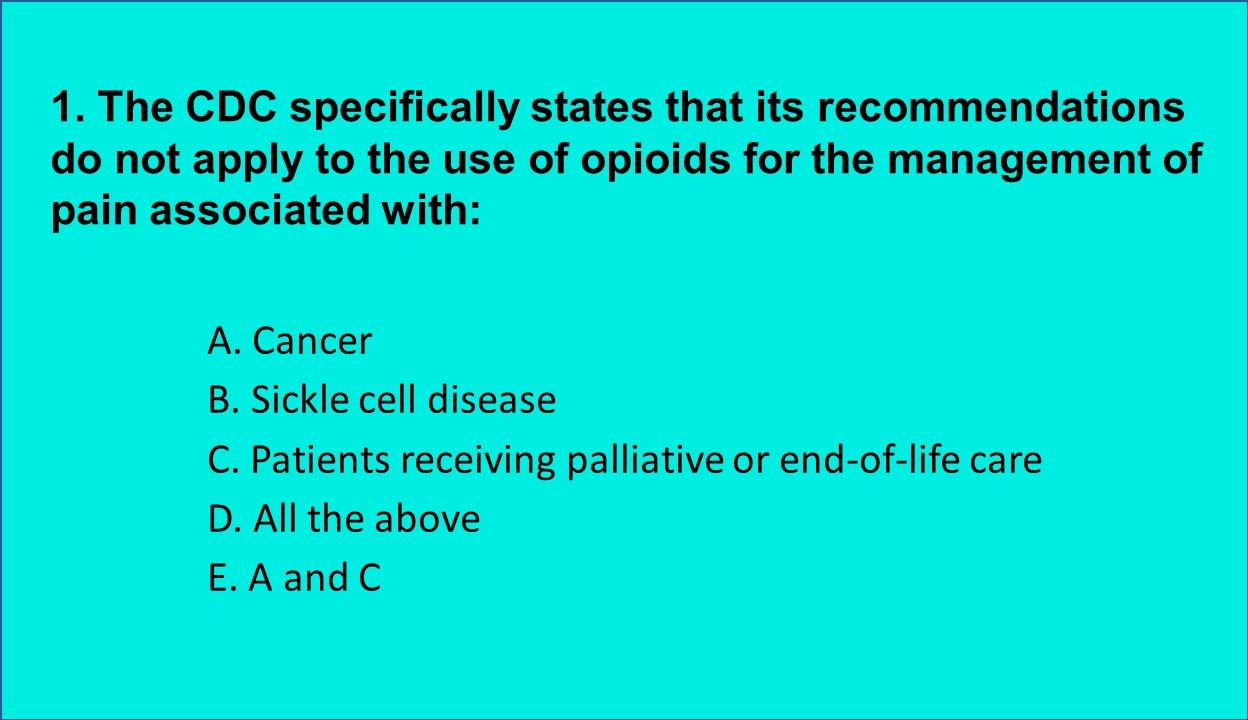
1. The CDC specifically states that its recommendations do not apply to the use of opioids for the management of pain associated with which of the above?
Answer: D. All the above. The guideline specifically notes that its recommendation do not apply to pain related to cancer or sickle cell disease or to those receiving palliative or end-of-life care.
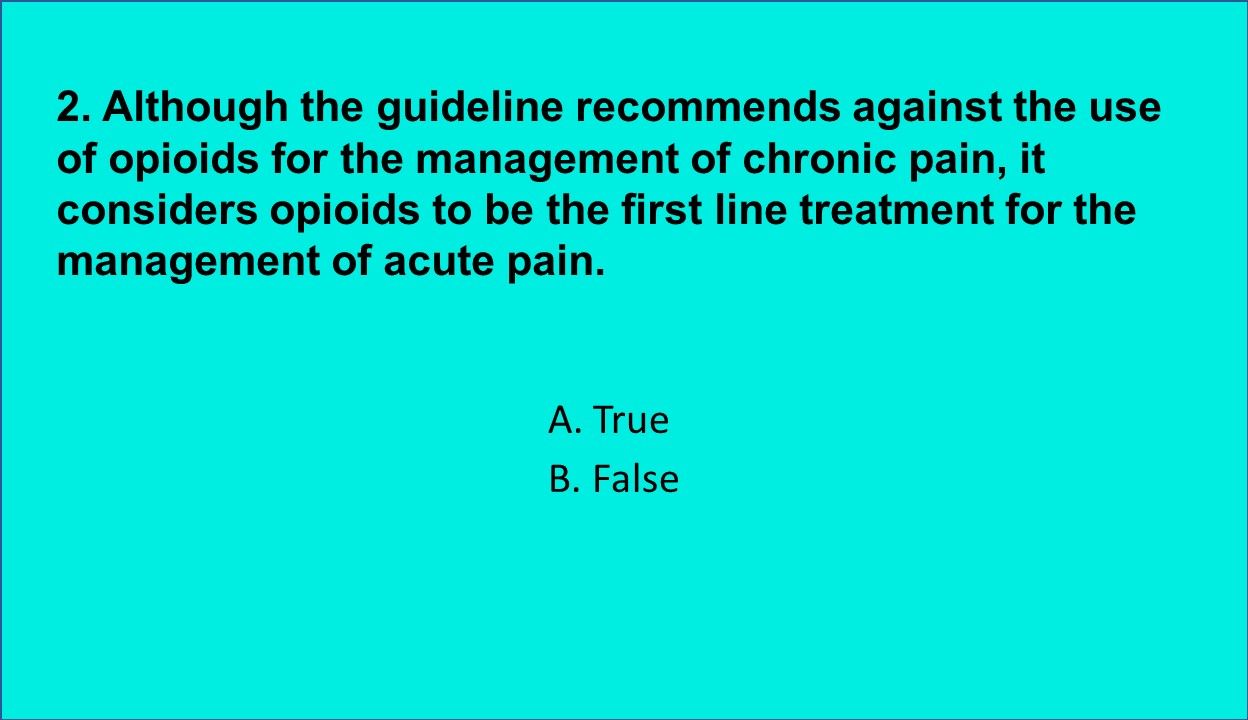
2. True or false: Although the guideline recommends against the use of opioids for the management of chronic pain, it considers opioids to be the first line treatment for the management of acute pain.
Answer: B. False. The guideline notes that nonopioid therapies including both nonpharmacologic and nonopioid pharmacologic therapies are as effective for the management of many types of acute pain as opioids and clinicians should consider these along with opioids.
- Medications: In many cases NSAIDs are more effective than opioids, especially for musculoskeletal pain.
- Nonpharmacologic therapies:Potential benefits are described for several including acupuncture, massage, and TENS.
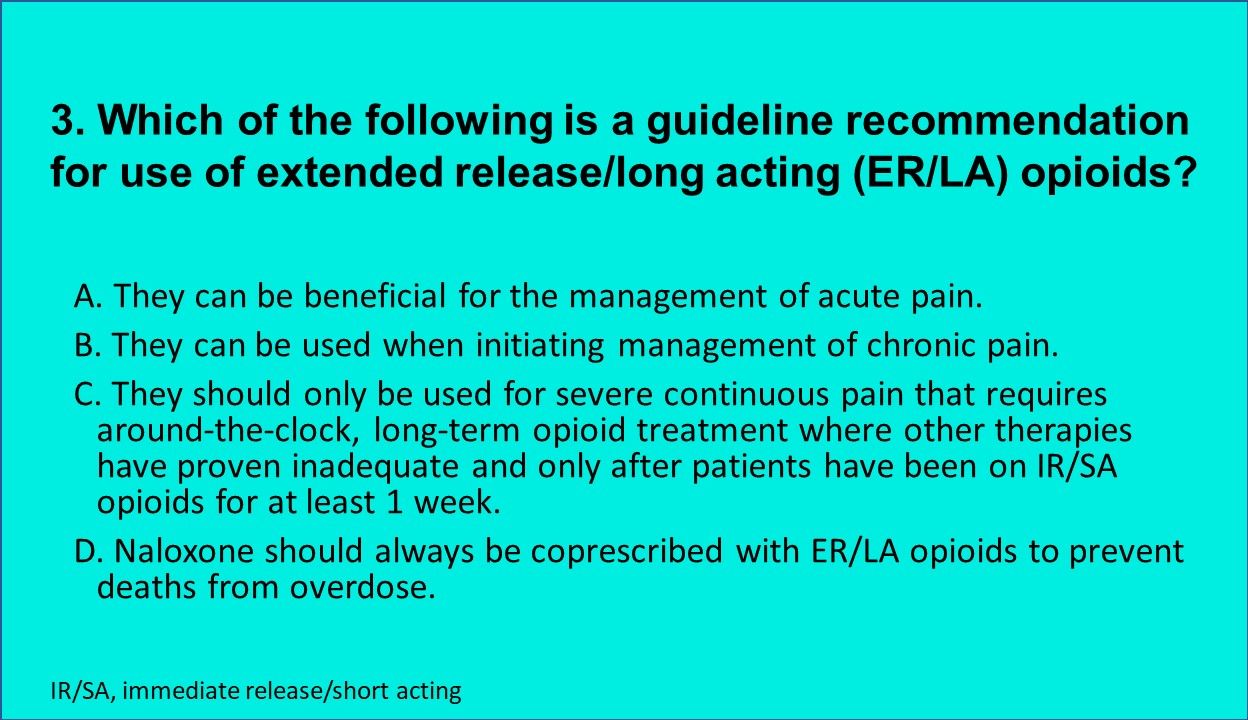
3. Which of the above is a guideline recommendation for use of extended release/long acting (ER/LA) opioids?
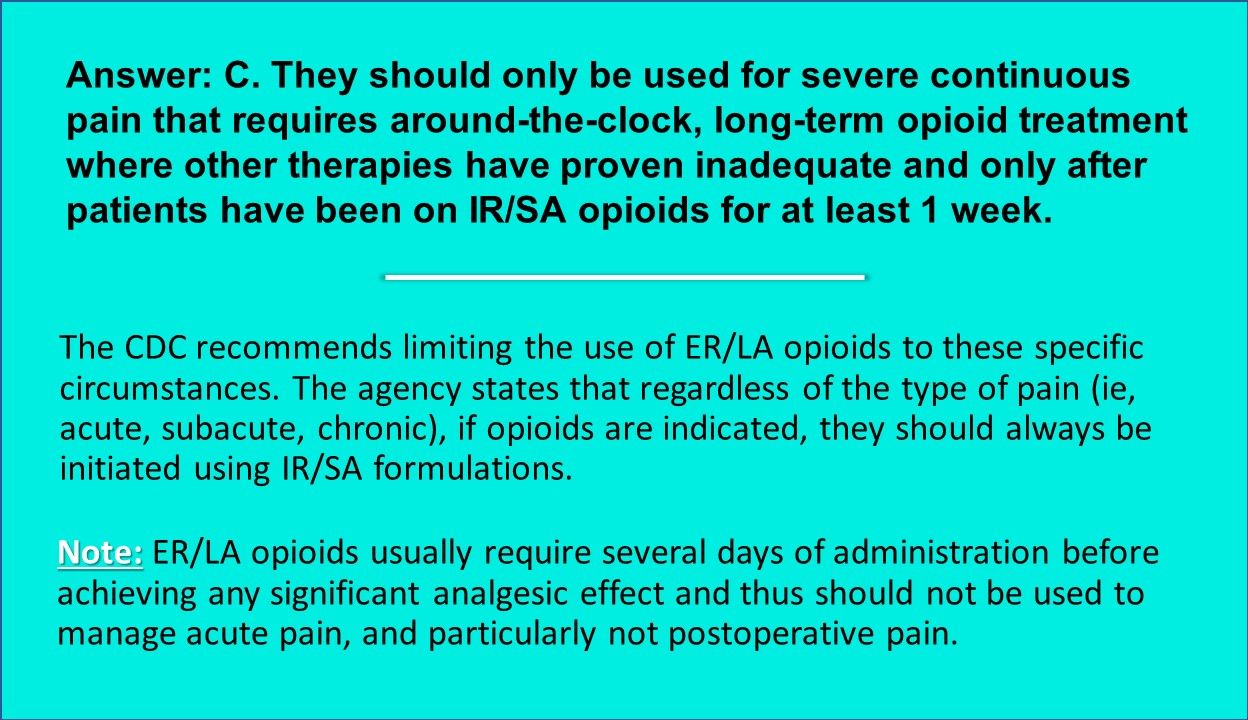
Answer: C. ER/LA opioids should only be used for severe continuous pain that requires around-the-clock, long-term opioid treatment where other therapies have proven inadequate and only after patients have been on IR/SA opioids for at least 1 week.
Note: ER/LA opioids usually require several days of administration before achieving any significant analgesic effect and thus should not be used to manage acute pain, and particularly not postoperative pain.
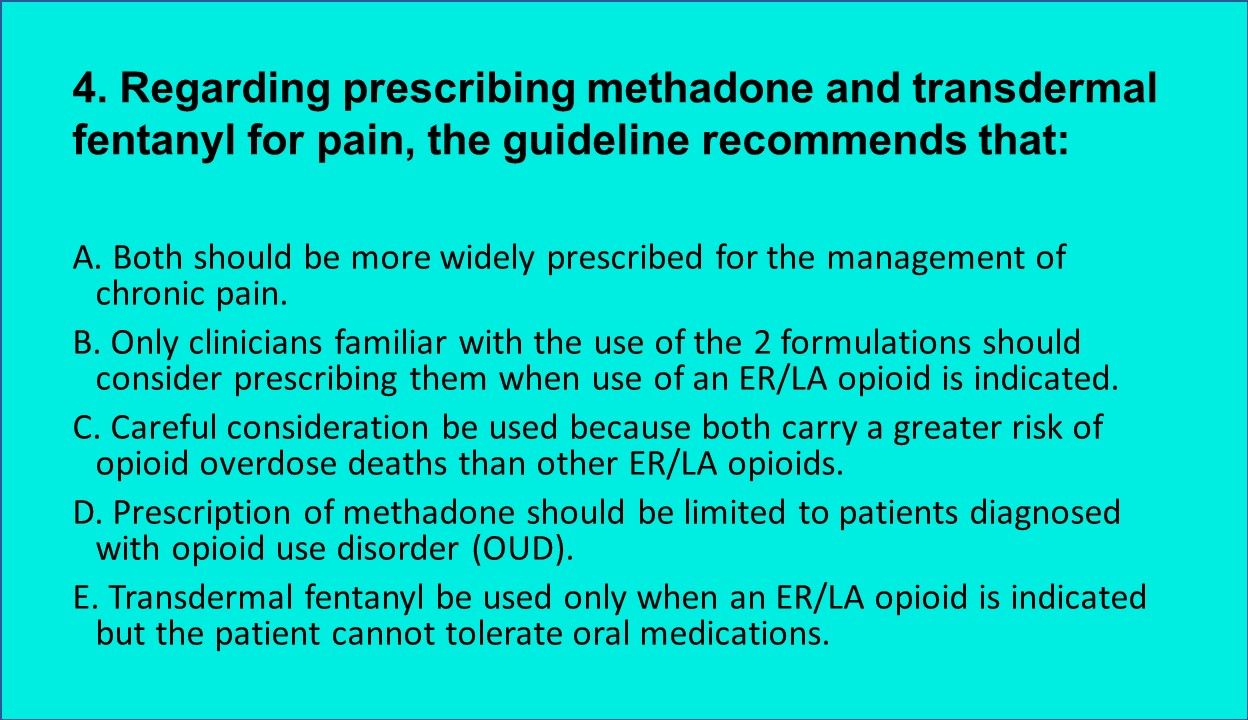
4. Regarding prescribing methadone and transdermal fentanyl for pain, the guideline recommends which of the above?
Answer: B. Only clinicians familiar with the use of the 2 formulations should consider prescribing them when use of an ER/LA opioid is indicated.
The guideline recommends that methadone and transdermal fentanyl prescribing be limited to clinicians familiar with their use because of their associated idiosyncratic adverse events:
- Methadone: Increased risk for QT prolongation.
- Transdermal fentanyl: Potential difficulties in determining appropriate dosage when switching from oral or parenteral opioids.
Author’s note: The recommendation seems somewhat odd as one would think that the prescription of any medications—especially those with a high risk of adverse events, such as opioids—should be limited to clinicians familiar with their use.
5. Which of the above do guideline authors suggest are among the factors that have led to use of opioids vs nonopioid alternatives to manage pain?
Answer: D. All the above. Inadequate clinician education and training in the management of pain and therapeutic options, insufficient access to a range of therapeutic alternatives, and insurance coverage and reimbursement issues have long been identified but unfortunately only limited steps have been taken to overcome them.
For example, the dearth of physician education on the management of pain—especially chronic pain—both during medical school and postgraduate training, has long been noted but continues to be a significant problem.
6. The guideline advises against prescribing which of the above classes of medications along with opioids?
Answer: C. Benzodiazepines. Combining opioids with benzodiazepines appears to significantly increase the risk of death from opioid overdoses primarily because both classes can cause respiratory depression. Also, while it appears that benzodiazepines do not provide any significant analgesic effect, they also can reduce the effectiveness of opioids. In contrast, SNRIs, gabapentinoids, and NSAIDs can all provide analgesia. There is growing concern, however, that using gabapentin with opioids may increase the risk of overdose death as a result of respiratory depression.
More on benzodiazepines and opioids: Although patients taking benzodiazepines long-term for anxiety or another mental disorder may require an opioid for severe acute pain, it is recommended that extended use be avoided unless there is no efficacious alternative available.
If a patient treated with opioids for chronic pain develops a mental health disorder where a benzodiazepine may be indicated, the CDC recommends psychotherapy and use of an agent such as buspirone or an antidepressant that has anxiolytic properties instead. It is important to remember that, like opioids, after extended use of benzodiazepines their dose needs to be tapered to avoid seizures and potentially death.
7. True or false? The guideline identified instruments with a high degree of accuracy for predicting which patients who are prescribed opioids who will go on to overdose or develop OUD.
Answer: B. False. The guideline committee was unable to identify any such predictive instrument, further underscoring the need for significant clinical judgement when considering initiating opioid therapy.
Current instruments used to evaluate risk of opioid misuse rely on history of substance abuse, which along with the presence of a mental disorder, are the only consistent factors predictive for developing problems with opioids. For all patients taking opioids, however, continued careful monitoring and reassessment are vital.
8. The CDC states in the guideline that the prescription of opioids is absolutely contraindicated for which group of patients?
Answer: F. None of the above. The CDC does note that extra caution and careful monitoring are required when prescribing opioids for each of these populations that are all at increased risk of developing serious adverse events from opioids.
9. True or false: If it is felt that after extended use of opioids the dose should be reduced or the medication discontinued, the guideline provided an optimal tapering schedule based on current research.
Answer: B. False. Although the CDC notes the importance of tapering opioids after extended use to prevent adverse events, it was unable to identify any single optimal tapering rate and states it should be individualized for each patient. This reflects the paucity of literature comparing various tapering schedules and the use of so-called “pain cocktails” where a long-acting opioid, usually liquid methadone, is combined with a syrup and based on dose equivalency, used to replace the opioid the patient is taking. The dose of the methadone is then gradually reduced and, although the patient is aware of the reduction, he is unaware of the dose which eliminates the psychological factors associated with fearing an exacerbation of the pain when a certain dosage level is reached.
More on tapering: The guideline authors note that buprenorphine may also be used as a substitute medication for patients who are unable to tolerate tapering. The advantage tapering with methadone is that it can be started immediately while with buprenorphine, because it is a partial agonist and can cause withdrawal in a patient taking a full agonist, initiation must be timed until the patient is in mild to moderate withdrawal from the opioid being discontinued.
Answer: C. Its recommendations should be considered to take precedence over state laws regarding prescription of opioids. The guideline does not state that it should take precedent over state laws regarding prescription of opioids. It is always important for clinicians to be aware of the applicable laws in their states as these vary from state to state.
Reference: Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain — United States, 2022. MMWR Recomm Rep 2022;71(No. RR-3):1–95. doi: http://dx.doi.org/10.15585/mmwr.rr7103a1
Related Content:





