© 2025 MJH Life Sciences™ , Patient Care Online – Primary Care News and Clinical Resources. All rights reserved.
Cystic Fibrosis and Personalized Medicine: A Brief History
These concise summaries outline key developments in the evolution of a promising genetics-based approach to cystic fibrosis treatment.
Personalized medicine, also known as precision medicine, continues to advance as a genetics-based approach to treating patients with cystic fibrosis (CF). In this approach, personalized interventions are applied for patients who have specific mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene. Scroll through the slides below to find concise summaries of key developments in the evolution of personalized, or precision, medicine for patients with CF.
A precise definition of precision medicine. Precision medicine is “an emerging approach for disease treatment and prevention that takes into account individual variability in genes, environment, and lifestyle for each person,” says the Precision Medicine Initiative. The approach may be used to more accurately predict which treatment and prevention strategies will work in which groups of patients rather than one in which strategies are developed with less consideration for differences between patients.
Treatment tailored to CF. Personalized medicine can enable doctors to tailor CF therapies to patients based on their genetic makeup. The existing CFTR modulator therapies-designed to correct the malfunctioning protein made by the CFTR gene-are ivacaftor (Kalydeco), lumacaftor/ivacaftor (Orkambi), tezacaftor/ivacaftor (Symdeko), and elexacaftor/tezacaftor/ivacaftor (Trikafta). More potential CFTR modulators are in development.
Altering the precision medicine landscape. Ivacaftor, the first drug that treated the underlying cause rather than the symptoms, was FDA approved in 2012 to treat the G551D CFTR gene variant that causes 3%-4% of CF cases. The FDA expanded the label to 9 additional mutations in 2014 and to 28 more in 2018, tripling eligibility to 14% of the CF population. In early studies, ivacaftor significantly decreased pulmonary morbidity, lowered hospitalization rates, and improved weight gain and quality of life. In a later study, CF-related hospital admissions decreased by 81%.
Orkambi doubles down. Orkambi (lumacaftor/ivacaftor), a CFTR potentiator and CFTR corrector combination for treating the underlying cause of CF in patients age ≥ 2 years with 2 copies of the F508del mutation in their CFTR gene (about half of CF cases), was first approved by the FDA in 2015. Participants in 2 double-blind, placebo-controlled clinical trials demonstrated improved lung function, reductions in pulmonary exacerbations, and improvements in body mass index.
Proof of concept. The development of ivacaftor and lumacaftor/ivacaftor, the first 2 CF drugs to gain FDA approval for clinical use, serves as proof-of-concept that targeting CFTR by modulators is a viable therapeutic option, according to the authors of a review published in the American Journal of Physiology Lung Cellular and Molecular Physiology on April 1, 2018. They noted, however, that these agents are known to be effective only in patients who have certain CFTR mutations, leaving many others without similar treatment options.
Breakthrough therapy. In 2019, the FDA granted approval to Trikafta (elexacaftor/ivacaftor/tezacaftor), the first triple combination therapy for patients with the most common CF mutation. Trikafta is approved for patients aged ≥12 years who have at least 1 F508del mutation in the CFTR gene (an estimated 90% of the CF population). The approval was based on study results in the New England Journal of Medicine published November 7, 2019 that showed elexacaftor–tezacaftor–ivacaftor to be efficacious in patients with Phe508del–minimal function genotypes in whom previous CFTR modulator regimens were ineffective.
Ongoing challenges. TCTs promise to offer benefit for most patients with CF but face several challenges according to a review published November 12, 2019 in Pediatric Pulmonology. A subset of patients may not exhibit pronounced benefit or could experience adverse effects that limit their ability to tolerate the treatment. Refractory CFTR mutations in an estimated 10% of patients currently are not well addressed by TCTs or other CFTR modulators. Novel agents are being sought even as clinical trials are problematic for persons whose mutations are rare.
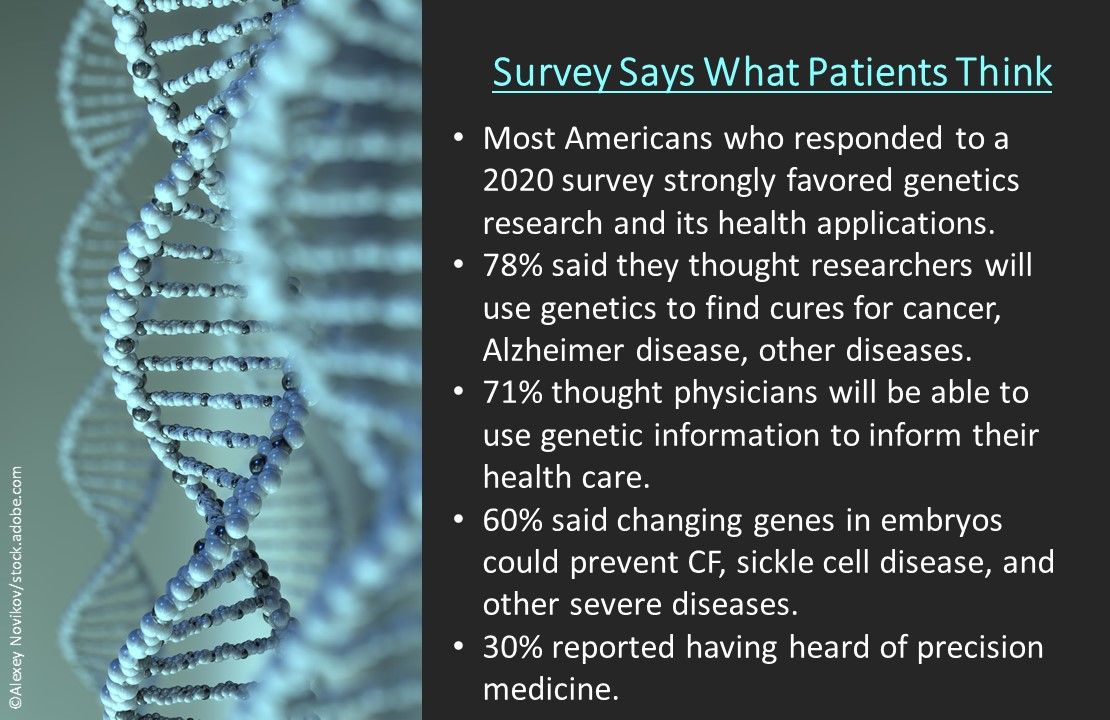
Survey says what patients think. Americans strongly favored genetics research and its health applications in a January 2020 survey released by the American Society of Human Genetics in partnership with Research!America. Respondents said they thought researchers will use genetics to find cures for cancer, Alzheimer disease, and other diseases (78%); physicians will be able to use genetic information to inform their health care (71%); and changing genes in embryos could prevent CF, sickle cell disease, and other severe diseases (60%). Thirty percent reported having heard of precision medicine.